Fibrinogen Deficiency
Persistent fibrinogen deficiency can lead to bleeding complications and an increased risk in mortality. Early identification and treatment of fibrinogen deficiency could therefore save lives.
Correct perioperative management of fibrinogen loss experienced during heart surgery and postpartum haemorrhage is key to treatment success.
Fibrinogen role in haemostasis
Fibrinogen (Factor I) has many functions in haemostasis, a process that stops bleeding from damaged tissue. Such functions include coagulation (the creation of blood clots), fibrinolysis (the breaking down of blood clots), wound healing, inflammation and cell–cell interactions.
Role for fibrinogen in coagulation
Coagulation, or blood clotting, is a highly regulated process that can be separated into four distinct stages (Monroe and Hoffman et al., 2007) (Figure 1):
- initiation; the sensing of damaged tissue
- amplification; signalling to factors required for clot formation
- propagation; initiating clot formation
- stabilisation; completing clot formation
Figure 1. The key stages of the coagulation cascade (Adapted from Monroe and Hoffman et al., 2007). TF, tissue factor; vWF, von Willebrand factor.
Fibrinogen plays an important structural role in both the propagation and stabilisation stages of coagulation, allowing for both clot formation and stability. An important feature of the coagulation process is its ability to trigger a fast response when tissue is damaged. As a result, fibrinogen is produced in an inactive state (like many other coagulation factors) by the liver and is secreted into blood to a normal variable range described as 2–4.5 g/L (Collins et al., 2014) or 1.5–3.5 g/L (Tennent et al., 2007; Neerman-Arbez & Casini, 2018).
In its inactive state, fibrinogen is a large, soluble, hexameric glycoprotein that is made up of two copies each of three peptides Aα, Bβ and γ that are held together by disulphide bonds (Figure 2).
Figure 2. Fibrinogen structure; Purple = alpha chain, green = beta chain, red = gamma chain. (Adapted from Nacca et al., 2016).
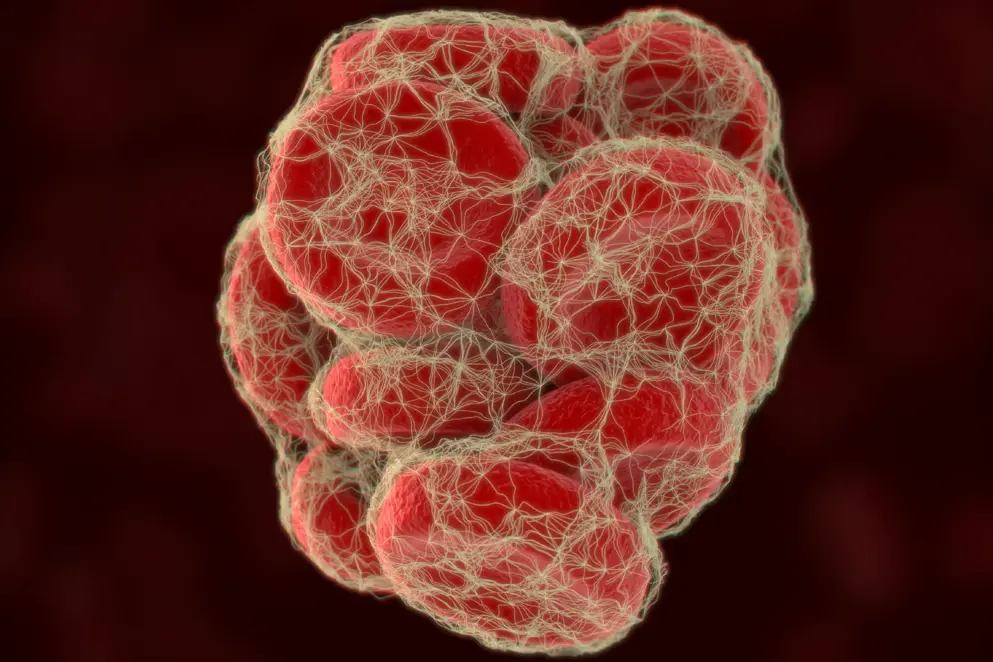
Upon initiation and amplification of the coagulation cascade (Figure 1), thrombin interacts with fibrinogen and cleaves the end-terminal regions of the Aα and Bβ peptides to produce fibrinopeptides A and B, respectively. This converts fibrinogen into soluble fibrin monomers that rapidly aggregate to form an insoluble fibrin polymer mesh. At the same time, thrombin converts another procoagulant, Factor XIII, into its active form, Factor XIIIa, a transglutaminase that cross-links glutamine residues from one fibrin monomer to lysine residues of another fibrin monomer, allowing for structural stability (Monroe and Hoffman et al., 2007) (Figure 3).
Figure 3. Fibrin polymers are stabilised by inter-monomer crosslinks catalysed by activated Factor XIII (Factor XIIIa) (Adapted from Adam et al., 2009).
Activated platelets aggregate on to the fibrin meshes through their surface glycoproteins IIb/IIIa and separately, bind to blood vessel walls to create a haemostatic plug (blood clot). Fibrin meshes also serve as a binding scaffold for other proteins involved in blood clotting (Laurens et al., 2006). This includes fibronectin (involved in cell adhesion), albumin (regulates fibrin ‘thickness’), thrombospondin (regulates the aggregation and binding of platelets to fibrin), Von Willebrand factor (involved in platelet adhesion) and fibrulin (promotes platelet adhesion to the extracellular matrix). Growth factors such as fibroblast growth factor-2 and vascular endothelial growth factor that encourage blood vessel repair also interact with fibrin meshes (Brown et al., 1996; Sahni et al., 1998). Finally, fibrin is involved in activating the immune response, the first line of defence upon tissue damage. This is achieved through fibrin binding and accumulating cells required for both an inflammatory response and for tissue repair (Esmon et al., 2012). Altogether, activated fibrinogen creates an adhesive and stable structure for building blood clots and promoting blood vessel repair.
Role for fibrinogen in clot degradation
Fibrin is involved in regulating fibrinolysis, a process whereby blood clots that are no longer needed are broken down. This action reduces circulating blood clots that have the potential to block vessels and cause further damage (Chapin & Hajjar, 2015).
Plasmin is a serine protease enzyme that inactivates various blood plasma proteins through enzymatic cleavage (proteolysis), including fibrin clots. Plasmin is produced and released from the liver as a zymogen called plasminogen and two circulating types exist based on the number of glycosylation moieties they possess (one versus two). Type I plasminogen, which contains two glycosylation moieties, is preferentially recruited to blood clots. Freely circulating plasminogen is normally inactive until it binds to an activator such as a blood clot. This allows for a conformational change that promotes plasminogen conversion to plasmin through enzymes such as tissue plasminogen activator (tPA) (Chapin & Hajjar, 2015) (Figure 4). Importantly, fibrin is a cofactor that allows tPA activity and therefore is involved in promoting plasmin formation (Hoylaerts et al., 1982; Horrevoets et al., 1997). If plasmin levels are too low, as occurs in the absence of fibrin, then blood clots may persist as they are not being efficiently broken down, thus increasing the risk of thrombosis. Indeed, roles for fibrinogen in both clot formation and breakdown is ‘paradoxical’ in nature, whereby a deficiency can lead to reduced blood clotting and excessive bleeding, but at the same time, increases the risk of thrombotic complications.
Figure 4. Activated fibrinogen (fibrin) plays an important role in plasmin-dependent clot degradation (Adapted from Kohler & Grant, 2000). t-PA, tissue plasminogen activator; u-PA, urokinase plasminogen activator; PAI-1, plasminogen activator inhibitor-1.
Fibrinogen dysregulation
The structural role for fibrinogen in clot formation and the regulatory role of fibrin in fibrinolysis impacts greatly on haemostasis, particularly during trauma involving bleeding. This is highlighted in patients that have congenital deficiencies of fibrinogen who are prone to excessive bleeding. Furthermore, fibrinogen is the first coagulant to dramatically decrease as a result of fibrinogen consumption, dilution or bleeding during trauma, cardiac surgery and postpartum haemorrhage.
of interest
are looking at
saved
next event
of interest
are looking at
saved
next event
Fibrinogen deficiency references
Abdul‐Kadir R, McLintock C, Ducloy A, El‐Refaey H, England A, Federici AB, et al. Evaluation and management of severe PPH. Transfusion. 2014;54:1756–68.
Adam SS, Key NS, Greenberg CS. D-dimer antigen: current concepts and future prospects. Blood. 2009;113;2878–87.
Asselta R, Duga S, Tenchini ML. The molecular basis of quantitative fibrinogen disorders. J Thromb Haemost. 2006;4(10):2115–29.
Belghiti J, Kayem G, Dupont C, Rudigoz R, Bouvier-Colle M, Deneux-Tharaux C et al. Oxytocin during labour and risk of severe postpartum haemorrhage: a population-based, cohort-nested case-control study. BMJ Open. 2011;1:e000514.
Besser MW, MacDonald SG. Acquired hypofibrinogenemia: current perspectives. J Blood Med. 2016;7:217–25.
Brennan SO, Wyatt J, Medicina D, Callea F, George PM. Fibrinogen brescia: hepatic endoplasmic reticulum storage and hypofibrinogenemia because of a gamma284 Gly—>Arg mutation. Am J Pathol. 2000;157:189–96.
Brennan SO, Maghzal G, Shneider BL, Gordon R, Magid MS, George PM. Novel fibrinogen gamma375 Arg—>Trp mutation (fibrinogen aguadilla) causes hepatic endoplasmic reticulum storage and hypofibrinogenemia. Hepatology. 2002;36:652–58.
Brennan SO, Davis RL, Conard K, Savo A, Furuya KN. Novel fibrinogen mutation γ314Thr→Pro (fibrinogen AI duPont) associated with hepatic fibrinogen storage disease and hypofibrinogenaemia. Liver Int. 2010;30:1541–47.
Brenner B. Haemostatic changes in pregnancy. Thrombosis Research. 2004;114:409–14.
Brown KJ, Maynes SF, Bezos A, Maguire DJ, Ford MD, Parish CR. A novel in vitro assay for human angiogenesis. Lab Invest. 1996;75:539–55.
Casini A, Neerman-Arbez M, Ariens RA, de Moerloose P. Dysfibrinogenemia: from molecular anomalies to clinical manifestations and management. J Thromb Haemost. 2015;13:909–19.
Casini A, de Moerloose P, Neerman-Arbez M. Clinical features and management of congenital fibrinogen deficiencies. Semin Thromb Hemost. 2016;42:366–74.
Casini A, Brungs T, Lavenu‐Bombled C, Vilar R, Neerman‐Arbez M, Moerloose P. Genetics, diagnosis and clinical features of congenital hypodysfibrinogenemia: a systematic literature review and report of a novel mutation. J Thromb Haemost. 2017;15:876–88.
Chapin JC, Hajjar KA. Fibrinolysis and the control of blood coagulation. Blood Rev. 2015;29:17–24.
Charbit B, Mandelbrot L, Samain E, Baron G, Haddaoui B, Keita H et al. The decrease of fibrinogen is an early predictor of the severity of postpartum haemorrhage. J Thromb Haemost. 2007;5:266–73.
Chauleur C, Cochery-Nouvellon E, Mercier E, Aya G, Fabbro-Peray P, Mismetti P et al. Some hemostasis variables at the end of the population distributions are risk factors for severe postpartum hemorrhages. J Thromb Haemost. 2008;6:2067–74.
Chee YE, Liu SE, Irwin MG. Management of bleeding in vascular surgery. British Journal of Anaesthesia. 2016;117:ii85–ii94.
Collins PW, Solomon C, Sutor K, et al. Theoretical modelling of fibrinogen supplementation with therapeutic plasma, cryoprecipitate, or fibrinogen concentrate. Br J Anaesth. 2014;113:585–95.
Cortet M, Deneux-Tharaux C, Dupont C, Colin C, Rudigoz RC, Bouvier-Colle MH, et al. Association between fibrinogen level and severity of postpartum haemorrhage: secondary analysis of a prospective trial. Br J of Anaesth. 2012;108:984–9.
de Bosch NB, Mosesson MW, Ruiz-Saez A, Echenagucia M, Rodriguez-Lemoin A. Inhibition of thrombin generation in plasma by fibrin formation (Antithrombin I). Thromb Haemost. 2002;88:253–58.
de Lloyd L, Bovington R, Kaye A, Collis RE, Rayment R, Sanders J et al. Standard haemostatic tests following major obstetric haemorrhage. International Journal of Obstetric Anesthesia. 2011;20:135–41.
de Moerloose P, Casini A, Neerman-Arbez M. Congenital fibrinogen disorders: an update. Semin Thromb Hemost. 2013;39:585–95.
Deneux-Tharaux C, Dupont C, Colin C, Rabilloud M, Touzet S, Lansac J et al. Multifaceted intervention to decrease the rate of severe postpartum haemorrhage: the PITHAGORE6 cluster-randomised controlled trial. BJOG. 2010;117:1278–87.
Dib N, Quelin F, Ternisien C, Hanss M, Michalak S, De Mazancourt P et al. Fibrinogen angers with a new deletion (gamma GVYYQ 346-350) causes hypofibrinogenemia with hepatic storage. J Thromb Haemost. 2007;5:1999–2005.
Esmon CT, Xu J, Lupu F. Innate immunity and coagulation. J Thromb Haemost. 2011;9:182–8.
Ferro D, Celestini A, Violi F. Hyperfibrinolysis in liver disease. Clin Liver Dis. 2009;13:21–31.
Franchini M, Lippi G. Fibrinogen replacement therapy: a critical review of literature. Blood Transfus. 2012;10:23–27.
Fries D, Martini WZ. Role of fibrinogen in trauma-induced coagulopathy. British Journal of Anaesthesia. 2010;105:116–21.
Fuchs RJ, Levin J, Tadel M, Merritt W. Perioperative coagulation management in a patient with afibrinogenemia undergoing liver transplantation. Liver Transpl. 2007;13:752–56.
Gielen C, Dekkers O, Stijnen T, Schoones J, Brand A, Klautz R et al. The effects of pre- and postoperative fibrinogen levels on blood loss after cardiac surgery: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. 2014;18:292–8.
Guasch E, Gilsanz F. Treatment of postpartum haemorrhage with blood products in a tertiary hospital: outcomes and predictive factors associated with severe haemorrhage. Clin Appl Thromb Hemost. 2016;22:685–92.
Hill MB, Brennan SO, Dear A, Strong J, Nejim T, Dolan G. Fibrinogen Nottingham II: a novel Bbeta Arg264gly substitution causing hypofibrinogenaemia. Thromb Haemost. 2006;96:378–80.
Hoffman M, Monroe DM. Coagulation 2006: a modern view on hemostasis. Hematol Oncol Clin North Am. 2007;21:1–11.
Horrevoets AJ, Pannekoek H, Nesheim ME. A steady-state template model that describes the kinetics of fibrin-stimulated [Glu1]- and [Lys78] plasminogen activation by native tissue-type plasminogen activator and variants that lack either the finger or kringle-2 domain. J Biol Chem. 1997;272:2183–91.
Hoylaerts M, Rijken DC, Lijnen HR, Collen D. Kinetics of the activation of plasminogen by human tissue plasminogen activator. Role of fibrin. J Biol Chem. 1982;257:2912–19.
Huissoud C, Carrabin N, Benchaib M, Fontaine O, Levrat A, Massingnon D et al. Coagulation assessment by rotation thrombelastometry in normal pregnancy. Thromb Haemost. 2009;101:755–61.
JPAC Transfusion Handbook (Joint United Kingdom [UK] Blood Transfusion and Tissue Transplantation Services Professional Advisory Committee). 2014. Available at: https://www.transfusionguidelines.org/transfusion-handbook/7-effective-transfusion-in-surgery-and-critical-care/7-3-transfusion-management-of-major-haemorrhage (accessed April 2019).
Karkouti K, McCluskey S, Syed S, Pazaratz C, Poonawala H, Crowther M. The influence of perioperative coagulation status on postoperative blood loss in complex cardiac surgery: A prospective observational study. Anesth Analg. 2010;110:1533–40.
Kassebaum NJ, Bertozzi-Villa A, Coggesshall MS. Global, regional, and national levels and causes of maternal mortality during 1990–2013; a systematic analysis for the Global Burden of Disease Study. Lancet. 2014;384:980–1004.
Kindo M, Hoang Minh T, Gerelli S, Perrier S, Meyer N, Schaeffer M et al. Plasma fibrinogen level on admission to the intensive care unit is a powerful predictor of postoperative bleeding after cardiac surgery with cardiopulmonary bypass. Thromb Res. 2014;134:360–8.
Kohler HP, Grant PJ. Plasminogen-activator inhibitor type 1 and coronary artery disease. N Engl J Med. 2000;15:1792–801.
Korte W, Feldges A. Increased prothrombin activation in a patient with congenital afibrinogenemia is reversible by fibrinogen substitution. Clin Investig. 1994;72:396–98.
Kozek-Langenecker SA, Ahmed AB, Afshari A, Albaladejo P, Aldecoa C, Barauskas G et al. Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology: First update 2016. Eur J Anaesthesiol. 2017;34:332–95.
Lak M, Keihani M, Elahi F, Peyvandi F, Mannucci PM. Bleeding and thrombosis in 55 patients with inherited afibrinogenaemia. Br J Haematol. 1999;107:204–06.
Levy JH, Tanaka KA, Steiner ME. Evaluation and management of bleeding during cardiac surgery. Curr Hematol Rep. 2005;4:368–72.
Liu J, Sun L, Wang J, Ji G. The relationship between fibrinogen and in-hospital mortality in patients with type A acute aortic dissection. Am J Emerg Med. 2018;36:741–4.
Laurens N, Koolwijk P, de Maat MP. Fibrin structure and wound healing. J Thromb Haemost. 2006;4:932–9.
Maegele M, Gu ZT, Huang QB, Yang H. Updated concepts on the pathophysiology and the clinical management of trauma hemorrhage and coagulopathy. Chin J Traumatol. 2017;20:125–32.
Makar M, Taylor J, Zhao M, Farrohi A, Trimming M, D’Attellis N et al. Perioperative coagulopathy, bleeding, and hemostasis during cardiac surgery: a comprehensive review. ICU Director. 2010;1:17–27.
Mosesson MW. Antithrombin I. Inhibition of thrombin generation in plasma by fibrin formation. Thromb Haemost. 2003;89:9–12.
Moulton MJ, Creswell LL, Mackey ME, Cox, JL, Rosenbloom M. Reexploration for bleeding is a risk factor for adverse outcomes after cardiac operations. J Thorac Cardiovasc Surg. 1996;111:1037–46.
Nacca CR, Shah KN, Truntzer JN, Rubin LE. Total knee arthroplasty in a patient with hypofibrinogenemia. Arthroplasty. 2016;2:177–82.
Neerman-Arbez, M., Casini, A. Clinical Consequences and Molecular Bases of Low Fibrinogen Levels. International Journal of Molecular Sciences. 2018;19:1.
Niepraschk-von Dollen K, Bamberg C, Henkelmann A, Mickley L, Kaufner L, Henrich W et al. Predelivery maternal fibrinogen as a predictor of blood loss after vaginal delivery. Arch Gynecol Obstet. 2016;294:745–51.
O'Riordan MN, Higgins JR. Haemostasis in normal and abnormal pregnancy. Best Pract Res Clin Obstet Gynaecol. 2003;17:385–96.
Oruc N, Tokat Y, Killi R, Tombuloglu M, Ilter T. Budd-Chiari syndrome in an afibrinogenemic patient: a paradoxical complication. Dig Dis Sci. 2006;51:378–80.
Palmer JD, Francis DA, Roath OS, Francis JL, Iannotti F. Hyperfibrinolysis during intracranial surgery: effect of high dose aprotinin. J Neurol Neurosurg Psychiatry. 1995;58:104–6.
Peyvandi F, DiMichele D, Bolton-Maggs PH, Lee CA, Tripodi A, Srivastava A. Classification of rare bleeding disorders (RBDs) based on the association between coagulant factor activity and clinical bleeding severity. J Thromb Haemost. 2012;10:1938–43.
Roberts I, Shakur H, Fawole B, Kuti M, Olayemi O, Bello A et al. Haematological and fibrinolytic status of Nigerian women with post-partum haemorrhage. BMC pregnancy and childbirth. 2018;18:143.
Sahni A, Odrljin T, Francis CW. Binding of basic fibroblast growth factor to fibrinogen and fibrin. J Biol Chem. 1998;273:7554–59.
Saner FH, Kirchner C. Monitoring and Treatment of Coagulation Disorders in End-Stage Liver Disease. Visc Med. 2016;32:241–48.
Scrutinio D, Giannuzzi P. Comorbidity in patients undergoing coronary artery bypass graft surgery: impact on outcome and implications for cardiac rehabilitation. European Journal of Preventative Cardiology. 2008;15:379–85.
Simon L, Santi TM, Sacquin P, Hamza J. Pre-anaesthetic assessment of coagulation abnormalities in obstetric patients: usefulness, timing and clinical implications. Br J Anaesth. 1997;78:678–83.
Tennent GA, Brennan SO, Stangou AJ, O’Grady J, Hawkins PN, Pepys MB. Human plasma fibrinogen is synthesised in the liver. Blood. 2007;109:1971–4.
Teufelsbauer H, Proidl S, Havel M, Vukovich T. Early activation of hemostasis during cardiopulmonary bypass: evidence for thrombin mediated hyperfibrinolysis. Thromb Haemost. 1992;68:250–2.
Theusinger OM, Wanner GA, Emmert MY, Billeter A, Eismon J, Seifert B et al. Hyperfibrinolysis diagnosed by rotational thromboelastometry (ROTEM) is associated with higher mortality in patients with severe trauma. Anesth Analg. 2011;113:1003–12.
Tziomalos K, Vakalopoulou S, Perifanis V, Garipidou V. Treatment of congenital fibrinogen deficiency: overview and recent findings. Vasc Health Risk Manag. 2009;5:843–8.
Venugopal A. Disseminated intravascular coagulation. Indian J Anaesth. 2014;58:603–8.
Vivacqua A, Koch CG, Yousuf AM, Nowicki ER, Houghtaling PL, Blackstone EH et al. Morbidity of bleeding after cardiac surgery: is it blood transfusion, reoperation for bleeding, or both? Ann Thorac Surg. 2011;91:1780–90.
Walden K, Jeppsson A, Nasic S, Backlund E, Karlsson M. Low Preoperative Fibrinogen Plasma Concentration Is Associated With Excessive Bleeding After Cardiac Operations. Ann Thorac Surg. 2014;97:1199–206.
Developed by EPG Health for Medthority in collaboration with CSL Behring, with content provided by CSL Behring.
Not intended for Healthcare Professionals outside Europe.

