Diabetic Kidney Disease: Challenges, Progress, and Possibilities
Diabetic Kidney Disease: Challenges, Progress, and Possibilities
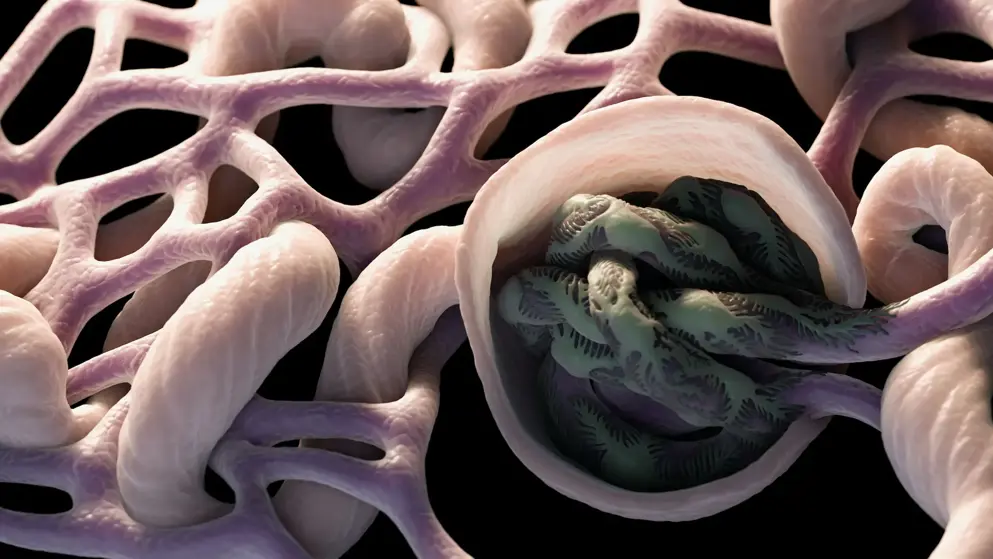
Diabetic kidney disease develops in approximately 40% of patients who are diabetic and is the leading cause of CKD worldwide. Although ESRD may be the most recognizable consequence of diabetic kidney disease, the majority of patients actually die from cardiovascular diseases and infections before needing kidney replacement therapy. The natural history of diabetic kidney disease includes glomerular hyperfiltration, progressive albuminuria, declining GFR, and ultimately, ESRD. Metabolic changes associated with diabetes lead to glomerular hypertrophy, glomerulosclerosis, and tubulointerstitial inflammation and fibrosis. Despite current therapies, there is large residual risk of diabetic kidney disease onset and progression. Therefore, widespread innovation is urgently needed to improve health outcomes for patients with diabetic kidney disease. Achieving this goal will require characterization of new biomarkers, designing clinical trials that evaluate clinically pertinent end points, and development of therapeutic agents targeting kidney-specific disease mechanisms (e.g., glomerular hyperfiltration, inflammation, and fibrosis). Additionally, greater attention to dissemination and implementation of best practices is needed in both clinical and community settings.
Read abstract on library site Access full article
Featured Learning Zones
You may be interested in...
Recent advancements in high-throughput sequencing have significantly enhanced our understanding of the genetics behind Cushing’s syndrome. Experts from the French Society of Endocrinology and French Society of Endocrinology and Pediatric Endocrinology reviewed genetic predispositions, resulting in a consensus statement on screening for Cushing disease and adrenal Cushing’s syndrome. Discover their key findings and recommendations.