First-Line Fibrinogen Concentrate for Bleeding Trauma
First-Line Administration of Fibrinogen Concentrate in the Bleeding Trauma Patient: Searching for Effective Dosages and Optimal Post-Treatment Levels Limiting Massive Transfusion - Further Results of the RETIC Study
Innerhofer N, Treichl B, Rugg C, Fries D, Mittermayr M, Hell T, et al. J Clin Med. 2021;10(17):3930.
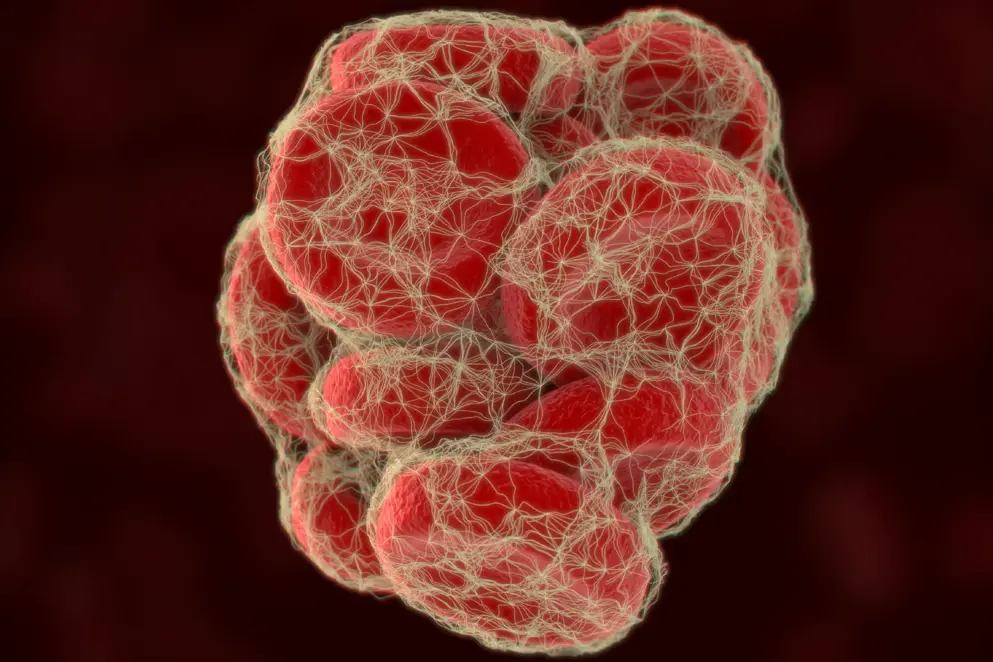
- Fibrinogen supplementation is recommended for treatment of severe trauma haemorrhage
- Secondary endpoint analysis showed that response to fibrinogen concentrate (FC) supplementation and the dosage needed depend on baseline fibrinogen levels
- Post-treatment fibrinogen concentrations also predict the need for massive transfusion: individualising baseline dose may increase efficacy of first-line FC administration in limiting blood loss
Fibrinogen supplementation is recommended for treatment of severe trauma haemorrhage: it is needed for stable clot formation and bleeding cessation, and is the first coagulation factor to reach critical thresholds during ongoing bleeding1.
The underlying evidence guiding the current European Guideline recommendations on fibrinogen supplementation dosing is low quality2
This analysis by Innerhofer and colleagues of a predefined secondary endpoint of the Reversal of Trauma-induced Coagulopathy using First-line Coagulation Factor Concentrates or Fresh-Frozen Plasma (RETIC) study provides additional data on how fibrinogen levels and fibrin polymerisation respond to first-line and rescue fibrinogen concentrate (FC) therapy. Primary endpoint results are published elsewhere3,4.
The RETIC study was a single-centre, parallel-group, open-label, randomised trial in 100 acute trauma patients (Injury Severity Score >15) with clinical signs of or a risk for substantial haemorrhage and thromboelastometry-diagnosed poor fibrin polymerisation (FibA10 <9 mm) and/or prolonged initiation of coagulation (ExTEM CT >90 s). First-line therapy was standardised body weight-dependent coagulation factor concentrates (mainly FC, n = 50) or fresh frozen plasma (FFP, n = 44). Twenty-three patients received FC as rescue therapy when double-dose FFP failed to correct coagulopathy (complete data available for 20)3.
Figure 1. Change in fibrinogen concentration (FC) in patients successfully treated with (A) a single dose (SD) of FC (5 [4–5] g, n = 38, median change 83 mg/dL or (B) a double dose (DD) of FC (10 [8–10] g, n = 12, median change 197 mg/dL). Respective changes in Fib10A are also shown (C, median change 4 mm; D, median change 4.5 mm). Outliers are marked as °.
A single dose of FC (median 62.5 [57–66.66] mg/kg) normalised fibrinogen and/or FibA10 values in patients with baseline fibrinogen >100 mg/dL and/or FibA10 >5 mm (post-treatment: median fibrinogen 213 mg/dL, FibA10 11 mm). Patients with lower baseline fibrinogen/Fib10A needed a second dose of FC to achieve normal fibrinogen/FibA10 values (Figure 1).
Post-treatment fibrinogen/Fib10A levels could predict the need for massive transfusion (MT, ≥10 units packed red blood cells within 24 hours). Compared with 37.9% (11/29) of patients below a threshold of slightly over 200 mg/dL fibrinogen (Fib10A 14 mm), only 12.2% (5/41) of patients above it needed MT (OR 4.35 [1.1627–20], P=0.0194).
Finally, FibA10 values were shown to correspond well with FibA30 values and fibrinogen plasma concentrations, validating its use as an early marker for therapeutic decision-making.
Overall, these findings show that effective FC supplementation depends on baseline deficiency and early normalisation of fibrinogen levels, and they support the target of 150–200 mg/dL as recommended by most European Guidelines.5 Early correction of fibrinogen deficiency with FC could reduce the subsequent need for MT.
Individual dosing to increase efficacy of first-line FC
- The response to FC supplementation and the dosage required to normalise fibrinogen/FibA10 values were dependent on baseline fibrinogen levels
- As post-treatment fibrinogen concentrations also predict the need for MT, baseline-adapted individual dosing may increase the efficacy of first-line FC administration in limiting blood loss
References
- Hiippala ST, Myllyla GJ, Vahtera EM. Hemostatic factors and replacement of major blood loss with plasma-poor red cell concentrates. Anesth Analg. 1995;81:360–365.q
- Spahn DR, Bouillon B, Cerny V, Duranteau J, Filipescu D, Hunt BJ, et al. The European Guideline on management of major bleeding and coagulopathy following trauma: fifth edition. Crit Care. 2019;23:98.
- Innerhofer P, Fries D, Mittermayr M, Innerhofer N, von Langen D, Hell T, et al. Reversal of Trauma-Induced Coagulopathy Using First-Line Coagulation Factor Concentrates or Fresh Frozen Plasma (RETIC): a single-centre, parallel-group, open-label, randomised trial. Lancet Haematol. 2017;4(6):e258–e271.
- Tauber H, Innerhofer N, von Langen D, Ströhle M, Fries D, Mittermayr M, et al. Dynamics of platelet counts in major trauma: the impact of haemostatic resuscitation and effects of platelet transfusion - a sub-study of the randomized controlled RETIC trial. J Clin Med. 2020;9(8):2420.
- Cěrný V, Maegele M, Agostini V, Fries D, Leal-Noval SR, Nardai G, et al. Variations and obstacles in the use of coagulation factor concentrates for major trauma bleeding across Europe: outcomes from a European Expert Meeting. Eur J Trauma Emerg Surg. 2021;1–12.
of interest
are looking at
saved
next event
Developed by EPG Health for Medthority in collaboration with CSL Behring, with content provided by CSL Behring.
Not intended for Healthcare Professionals outside Europe.

