Treatment
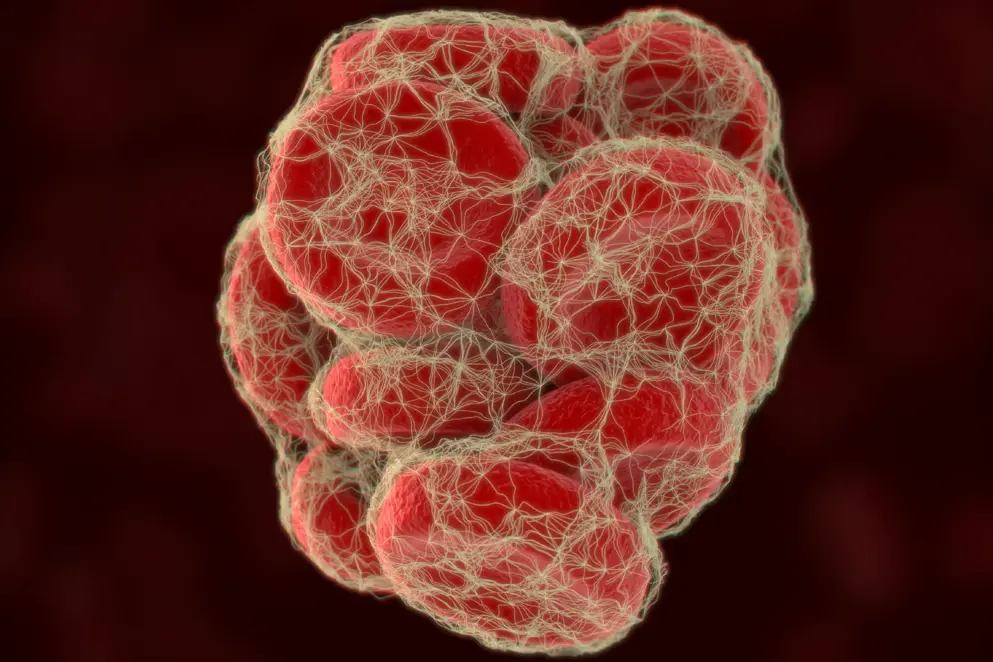
Depending on the strategy of volume resuscitation, it is often further diluted. Fibrinogen is also reduced (hypofibrinogenaemia), not detectable (afibrinogenaemia) and/or non-functional (dysfibrinogenaemia) in patients with congenital fibrinogen deficiencies. Since fibrinogen deficiencies are known to be associated with an increased risk of excessive bleeding and mortality, treatment involves fibrinogen replacement. Fibrinogen replacement therapies include fresh frozen plasma (FFP), cryoprecipitate and fibrinogen concentrate (FCH), which has been shown to be at least as effective as cryoprecipitate.
Fibrinogen concentrate is at least as effective as cryoprecipitate for treating fibrinogen deficiency; however, practical and safety differences exist.
Here, we highlight clinical trial data on fibrinogen replacement therapies for different clinical settings and introduce practical considerations comparing safety, storage and speed of delivery.
Fresh frozen plasma
Fresh frozen plasma (FFP) is the most commonly used source of coagulation factor replenishment. FFP is prepared by centrifugation of carefully obtained whole blood and contains fibrinogen at a variable concentration of 0.6 g/300mL unit or 2.0 g/L (range = 0.9 to 3.2 g/L), as well as albumin, protein C, protein S antithrombin and tissue factor pathway inhibitor (Theusinger et al., 2011; Kelley & Guzman, 2018). It is stored by freezing to less than -25°C within 8 hours of collection (Stanworth & Tinmouth, 2009).
FFP can be used to treat fibrinogen deficiencies; however, it has several limitations including a low fibrinogen concentration (Theusinger et al., 2011). Large volumes would therefore need to be administered in the case of severe hypofibrinogenemia, increasing the risk of transfusion related complications such as TRALI (transfusion-related acute lung injury) (Benson et al., 2009). It is therefore not recommended as a treatment option for fibrinogen replenishment and should only be used in the absence of cryoprecipitate or fibrinogen concentrate (Franchini & Lippi, 2012; McDonnell, 2018; Spahn et al., 2019).
of interest
are looking at
saved
next event
Treatment references
Abdul-Kadir R, McLintock C, Ducloy AS, El-Refaey H, England A, Federici AB et al. Evaluation and management of postpartum hemorrhage: consensus from an international expert panel. Transfusion. 2014;54:1756–68.
Ahmed S, Harrity C, Johnson S, Varadkar S, McMorrow S, Fanning R et al. The efficacy of fibrinogen concentrate compared with cryoprecipitate in major obstetric haemorrhage—an observational study. Transfus Med. 2012; 22: 344–9.
Akbari E, Safari S, Hatamabadi H. The effect of fibrinogen concentrate and fresh frozen plasma on the outcome of patients with acute traumatic coagulopathy: A quasi-experimental study. Am J Emerg Med. 2018;36:1947–1950.
Allard S, Green L, Hunt BJ. How we manage the haematological aspects of major obstetric haemorrhage. Br J Haematol. 2014;164:177–88.
Benson AB, Moss M, Silliman CC. Transfusion-related acute lung injury (TRALI): a clinical review with emphasis on the critically ill. British journal of haematology. 2009;147:431–43.
Bilecen S, Peelen LM, Kalkman CJ, Spanjersberg AJ, Moons KG, Nierich AP. Fibrinogen concentrate therapy in complex cardiac surgery. J Cardiothorac Vasc Anesth. 2013;27:12–7.
Bilecen S, de Groot JA, Kalkman CJ, Spanjersberg AJ, Bruinsma BB, Moons KG et al. Effect of fibrinogen concentrate on intraoperative blood loss among patients with intraoperative bleeding during high-risk cardiac surgery: a randomized clinical trial. JAMA. 2017;317:738–47.
Bornikova L, Peyvandi F, Allen G, Bernstein J, Manco-Johnson MJ. Fibrinogen replacement therapy for congenital fibrinogen deficiency. J Thromb Haemost. 2011;9:1687–704.
Casini A, de Moerloose P, Neerman-Arbez M. Clinical features and management of congenital fibrinogen deficiencies. Semin Thromb Hemost. 2016;42:366–74.
Chauleur C, Cochery-Nouvellon E, Mercier E, Aya G, Marès P, Mismetti P et al. Analysis of the venous thromboembolic risk associated with severe postpartum haemorrhage in the NOHA First cohort. Thromb Haemost. 2008;100:773–9.
Charbit B, Mandelbrot L, Samain E, Baron G, Haddaoui B, Keita H et al. The decrease of fibrinogen is an early predictor of the severity of postpartum haemorrhage. J Thromb Haemost. 2007;5:266–73.
Colavecchia AC, Cohen DA, Harris JE, Thomas JM, Lindberg S, Leveque C et al. Impact of intraoperative factor concentrates on blood product transfusions during orthotopic liver transplantation. Transfusion. 2017;57:3026–34.
Collins PW, Solomon C, Sutor K, et al. Theoretical modelling of fibrinogen supplementation with therapeutic plasma, cryoprecipitate, or fibrinogen concentrate. Br J Anaesth. 2014;113:585–595.
Collins P, Abdul-Kadir R, Thachil J; Subcommittees on Women' s Health Issues in Thrombosis and Haemostasis and on Disseminated Intravascular Coagulation. Management of coagulopathy associated with postpartum hemorrhage: guidance from the SSC of the ISTH. J Thromb Haemost. 2016;14:205–10.
Collins PW, Cannings-John R, Bruynseels D, Mallaiah S, Dick J, Elton C et al. Viscoelastometric-guided early fibrinogen concentrate replacement during postpartum haemorrhage: OBS2, a double-blind randomized controlled trial. Br J Anaesth. 2017;119:411–21.
Cortet M, Deneux-Tharaux C, Dupont C, Colin C, Rudigoz RC, Bouvier-Colle MH, et al. Association between fibrinogen level and severity of postpartum haemorrhage: secondary analysis of a prospective trial. Br J of Anaesth. 2012;108:984–9.
Costa-Filho R, Hochleitner G, Wendt M, Teruya A, Spahn DR. Over 50 years of fibrinogen concentrate. Clin Appl Thromb Hemost. 2016;22:109–14.
Curry N, Foley C, Wong H, Mora A, Curnow E, Zarankaite A et al. Early fibrinogen concentrate therapy for major haemorrhage in trauma (E-FIT 1): results from a UK multi-centre, randomised, double blind, placebo-controlled pilot trial. Crit Care. 2018;22:164.
De Lorenzo C, Calatzis A, Welsch U, Heindl B. Fibrinogen concentrate reverses dilutional coagulopathy induced in vitro by saline but not by hydroxyethyl starch 6%. Anesth Analg. 2006;102:1194–1200.
Di Nisio M, Baudo F, Cosmi B, D'Angelo A, De Gasperi A, Malato A et al. Diagnosis and treatment of disseminated intravascular coagulation: guidelines of the Italian Society for Haemostasis and Thrombosis (SISET). Thromb Res. 2012;129:e177–84.
Downey LA, Andrews J, Hedlin H, Kamra K, McKenzie ED, Hanley FL et al. Fibrinogen concentrate as an alternative to cryoprecipitate in a postcardiopulmonary transfusion algorithm in infants undergoing cardiac surgery. Anesth Analg. 2019;doi:10.1213/ANE.0000000000004384.
European Association for the Study of the Liver. EASL Clinical Practical Guidelines on the management of acute (fulminant) liver failure. J Hepatol. 2017;66:1047–1081.
Fassl J, Lurati Buse G, Filipovic M, Reuthebuch O, Hampl K, Seeberger MD et al. Perioperative administration of fibrinogen does not increase adverse cardiac and thromboembolic events after cardiac surgery. Br J Anaesth. 2015;114:225–34.
Fenger-Eriksen C, Jensen TM, Kristensen BS, Jensen KM, Tonnesen E, Ingerslev J et al. Fibrinogen substitution improves whole blood clot firmness after dilution with hydroxyethyl starch in bleeding patients undergoing radical cystectomy: a randomized, placebo-controlled clinical trial. J Thromb Haemost. 2009;7:795–802.
Fominskiy E, Nepomniashchikh VA, Lomivorotov VV, Monaco F, Vitiello C, Zangrillo A et al. Efficacy and Safety of Fibrinogen Concentrate in Surgical Patients: A Meta-Analysis of Randomized Controlled Trials. J Cardiothorac Vasc Anesth. 2016;30:1196–204.
Franchini M, Lippi G. Fibrinogen replacement therapy: a critical review of the literature. Blood Transfus. 2012;10:23–7.
Fries D, Krismer A, Klingler A, Streif W, Klima G, Wenzel V et al. Effect of fibrinogen on reversal of dilutional coagulopathy: a porcine model. Br J Anaesth. 2005;95:172–7.
Fries D, Innerhofer P, Reif C, Streif W, Klingler A, Schobersberger W et al. The effect of fibrinogen substitution on reversal of dilutional coagulopathy: an in vitro model. Anesth Analg. 2006;102:347–51.
Frith D, Goslings JC, Gaarder C, Maegele M, Cohen MJ, Allard S et al. Definition and drivers of acute traumatic coagulopathy: clinical and experimental investigations. J Thromb Haemost. 2010;8:1919–25.
Galas F, Almeida JP, Fukushima JT, Vincent JL, Osawa EA, Zeferino S et al. Hemostatic effects of fibrinogen concentrate compared with cryoprecipitate in children after surgery: a randomised pilot trial. J Thorac Cardiovasc Surg. 2014;148:1647– 55.
Gayat E, Resche-Rigon M, Morel O, Possignol M, Mantz J, Nicolas-Robin A et al. Predictive factors of advanced interventional procedures in a multicentre severe postpartum haemorrhage study. Intensive Care Med. 2011;37:1816–25.
Giordano P, Luciani M, Grassi M, De Leonardis F, Coletti V, Santoro N. Supplementation of fibrinogen concentrate in children with severe acquired hypofibrinogenaemia during chemotherapy for acute lymphoblastic leukaemia: our experience. Blood Transfus. 2014;12:s156–7.
Groeneveld DJ, Adelmeijer J, Hugenholtz GC, Ariëns RA, Porte RJ, Lisman T. Ex vivo addition of fibrinogen concentrate improves the fibrin network structure in plasma samples taken during liver transplantation. J Thromb Haemost. 2015;13:2192–201.
Guasch E, Gilsanz F. Treatment of postpartum hemorrhage with blood products in a tertiary hospital: outcomes and predictive factors associated with severe hemorrhage. Clin Appl Thromb Hemost. 2016;22:685–92.
Haas T, Fries D, Velik-Salchner C, Reif C, Klingler A, Innerhofer P. The in vitro effects of fibrinogen concentrate, factor XIII and fresh frozen plasma on impaired clot formation after 60% dilution. Anesth Analg. 2008;106:1360–5.
Haas T, Spielmann N, Restin T, Seifert B, Henze G, Obwegeser J et al. Higher fibrinogen concentrations for reduction of transfusion requirements during major paediatric surgery: A prospective randomised controlled trial. Br J Anaesth. 2015;115:234–43.
Huissoud C, Carrabin N, Benchaib M, Fontaine O, Levrat A, Massingnon D et al. Coagulation assessment by rotation thrombelastometry in normal pregnancy. Thromb Haemost. 2009;101:755–61.
Idris SF, Hadjinicolaou AV, Sweeney M, Winthrop C, Balendran G, Besser M. The efficacy and safety of cryoprecipitate in the treatment of acquired hypofibrinogenaemia. Br J Haematol. 2014;166:458–61.
Innerhofer P, Fries D, Mittermayr M, Innerhofer N, von Langen D, Hell T et al. Reversal of trauma-induced coagulopathy using first-line coagulation factor concentrates or fresh frozen plasma (RETIC): a single-centre, parallel-group, open-label, randomised trial. Lancet Haematol. 2017;4:e258–71.
Itagaki Y, Hayakawa M, Maekawa K, Saito T, Kodate A, Honma Y et al. Early administration of fibrinogen concentrate is associated with improved survival among severe trauma patients: a single-centre propensity score-matched analysis. World J Emerg Surg. 2020;15:7. doi: 10.1186/s13017-020-0291-9.
Kaspereit F, Doerr B, Dickneite G. The effect of fibrinogen concentrate administration on coagulation abnormalities in a rat sepsis model. Blood Coagul Fibrinolysis. 2004;15:39–43.
Karkouti K, Callum J, Crowther MA, McCluskey SA, Pendergrast J, Tait G et al. The relationship between fibrinogen levels after cardiopulmonary bypass and large volume red cell transfusion in cardiac surgery: an observational study. Anesth Analg. 2013;117:14–22.
Karkouti K, Callum J, Rao V, Heddle N, Farkouh ME, Crowther MA, Scales DC. Protocol for a phase III, non-inferiority, randomised comparison of a new fibrinogen concentrate versus cryoprecipitate for treating acquired hypofibrinogenaemia in bleeding cardiac surgical patients: the FIBRES trial. BMJ Open. 2018:e020741. doi: 10.1136/bmjopen-2017-020741.
Karlsson M, Ternström L, Hyllner M, Baghaei F, Flinck A, Skrtic S et al. Prophylactic fibrinogen infusion reduces bleeding after coronary artery bypass surgery. A prospective randomised pilot study. Thromb Haemost. 2009;102:137–44.
Kelley W, Guzman N. Fresh Frozen Plasma (FFP). StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513347/ (accessed April 2019).
Kelly M, Waldhauser H, Vilchez T, Dlotko E, Hutcheson R. PSU8: Comparing costs of using fibrinogen concentrate versus fresh frozen plasma in the treatment of bleeding during cardiac surgery in the Netherlands. Value Heal. 2019;22:S893.
Kikuchi M, Itakura A, Miki A, Nishibayashi M, Ikebushi K, Ishihara O. Fibrinogen concentrate substitution therapy for obstetric hemorrhage complicated by coagulopathy. J Obstet Gynaecol Res. 2013;39:770–6.
Kindo M, Hoang Minh T, Gerelli S, Perrier S, Meyer N, Schaeffer M et al. Plasma fibrinogen level on admission to the intensive care unit is a powerful predictor of postoperative bleeding after cardiac surgery with cardiopulmonary bypass. Thromb Res. 2014;134:360–368.
Kozek-Langenecker SA, Ahmed AB, Afshari A, Albaladejo P, Aldecoa C, Barauskas G et al. Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology: first update 2016. Eur J Anaesthesiol. 2017;34:332–95.
Kreuz W, Meili E, Peter-Salonen K, Haertel S, Devay J, Krzensk U et al. Efficacy and tolerability of a pasteurised human fibrinogen concentrate in patients with congenital fibrinogen deficiency. Transfus Apher Sci. 2005;32:247–53.
Kwapisz MM, Kent B, DiQuinzio C, LeGare J, Garnett S, Swyer W et al. The prophylactic use of fibrinogen concentrate in high‐risk cardiac surgery. Acta Anaesthesiol Scand. 2020;aas.13540.
Lancé MD, Ninivaggi M, Schols SE, Feijge MA, Oehrl SK, Kuiper GJ et al. Perioperative dilutional coagulopathy treated with fresh frozen plasma and fibrinogen concentrate: a prospective randomized intervention trial. Vox Sang. 2012;103:25–34.
Levi M, Toh CH, Thachil J, Watson HG. Guidelines for the diagnosis and management of disseminated intravascular coagulation. Br J Haematol. 2009;145:24–33.
Li J, Gong J, Zhu F, Moodie J, Newitt A, Uruthiramoorthy L et al. Fibrinogen concentrate in cardiovascular surgery: A meta-analysis of randomized controlled trials. Anesthesia & Analgesia. 2018;127:612–21.
Lunde J, Stensballe J, Wikkelsø A, Johansen M, Afshari A. Fibrinogen concentrate for bleeding--a systematic review. Acta Anaesthesiol Scand. 2014;58:1061–74.
Makino S, Takeda S, Kobayashi T, Murakami M, Kubo T, Hata T et al. National survey of fibrinogen concentrate usage for post-partum hemorrhage in Japan: Investigated by the Perinatology Committee, Japan Society of Obstetrics and Gynecology. J Obstet Gynaecol Res. 2015;41:1155–60.
Mallaiah S, Barclay P, Harrod I, Chevannes C, Bhalla A. Introduction of an algorithm for ROTEM-guided fibrinogen concentrate administration in major obstetric haemorrhage. Anaesthesia. 2015;70:166–175.
Manco-Johnson MJ, Dimichele D, Castaman G, Fremann S, Knaub S, Kalina U et al. Pharmacokinetics and safety of fibrinogen concentrate. J Thromb Haemost. 2009;7:2064–9.
Mathijssen IM. Guideline for care of patients with the diagnoses of craniosynostosis: working group on craniosynostosis. J Craniofac Surg. 2015;26:1735–807.
Matsunaga S, Takai Y, Nakamura E, Era S, Ono Y, Yamamoto K et al. The clinical efficacy of fibrinogen concentrate in massive obstetric haemorrhage with hypofibrinogenaemia. Sci Rep. 2017;7:46749. doi: 10.1038/srep46749.
McDonnell NJ. How to replace fibrinogen in postpartum haemorrhage situations? (Hint: Don't use FFP!). International Journal of Obstetric Anesthesia. 2018;33:4–7.
Mengoli C, Franchini M, Marano G, Pupella S, Vaglio S, Marietta M et al. The use of fibrinogen concentrate for the management of trauma-related bleeding: a systematic review and meta-analysis. Blood Transfus. 2017;15:318–24.
Mittermayr M, Streif W, Haas T, Fries D, Velik-Salchner C, Klingler A et al. Hemostatic changes after crystalloid or colloid fluid administration during major orthopedic surgery: the role of fibrinogen administration. Anesth Analg. 2007;105:905–17.
Najafi A, Shariat Moharari R, Orandi AA, Etezadi F, Sanatkar M, Khajavi MR. Prophylactic administration of fibrinogen concentrate in perioperative period of total hip arthroplasty: a randomized clinical trial study. Acta Med Iran. 2014;52:804–10.
Nascimento B, Goodnough LT, Levy JH. Cryoprecipitate therapy. Br J Anaesth. 2014;113:922–34.
Nascimento B, Callum J, Tien H, Peng H, Rizoli S, Karanicolas P et al. Fibrinogen in the initial resuscitation of severe trauma (FiiRST): a randomized feasibility trial. Br J Anaesth. 2016;117:775–782.
NICE guideline NG24. Transfusion: blood transfusion. Methods, evidence and recommendations. November 2015. Available at: https://www.ncbi.nlm.nih.gov/books/NBK327570/pdf/Bookshelf_NBK327570.pdf
Nienaber U, Innerhofer P, Westermann I, Schöchl H, Attal R, Breitkopf R et al. The impact of fresh frozen plasma vs coagulation factor concentrates on morbidity and mortality in trauma-associated haemorrhage and massive transfusion. Injury. 2011;42:697–701.
Noval-Padillo JA, León-Justel A, Mellado-Miras P, Porras-Lopez F, Villegas-Duque D, Gomez-Bravo MA et al. Introduction of fibrinogen in the treatment of hemostatic disorders during orthotopic liver transplantation: implications in the use of allogenic blood. Transplant Proc. 2010;42:2973–74.
Okerberg CK, Williams LA 3rd, Kilgore ML, Kim CH, Marques MB, Schwartz J et al. Cryoprecipitate AHF vs. fibrinogen concentrates for fibrinogen replacement in acquired bleeding patients - an economic evaluation. Vox Sang. 2016;111:292–8.
Peyvandi F. Results of an international, multicentre pharmacokinetic trial in congenital fibrinogen deficiency. Thromb Res. 2009;124:S9–11.
Poujade O, Zappa M, Letendre I, Ceccaldi PF, Vilgrain V, Luton D. Predictive factors for failure of pelvic arterial embolization for postpartum hemorrhage. Int J Gynaecol Obstet. 2012;117:119–23.
Rahe-Meyer N, Pichlmaier M, Haverich A, Solomon C, Winterhalter M, Piepenbrock S et al. Bleeding management with fibrinogen concentrate targeting a high-normal plasma fibrinogen level: a pilot study. Br J Anaesth. 2009;102:785–792.
Rahe-Meyer N, Hanke A, Schmidt DS, Hagl C, Pichlmaier M. Fibrinogen concentrate reduces postoperative bleeding when used as first-line hemostatic therapy during major aortic replacement surgery: results from a randomized, placebo-controlled trial. J Thorac Cardiovasc Surg. 2013a;145:S178–S185.
Rahe-Meyer N, Solomon C, Hanke A, Schmidt DS, Knoerzer D, Hochleitner G et al. Effects of fibrinogen concentrate as first-line therapy during major aortic replacement surgery: a randomized, placebo-controlled trial. Anesthesiology. 2013b;118:40–50.
Rahe-Meyer N, Levy JH, Mazer CD, Schramko A, Klein AA, Brat R et al. Randomized evaluation of fibrinogen vs placebo in complex cardiovascular surgery (REPLACE): a double-blind phase III study of haemostatic therapy. Br J Anaesth. 2016;117:41–51.
Rahe-Meyer N, Levy JH, Mazer CD, Schramko A, Klein AA, Brat R et al. Randomized evaluation of fibrinogen versus placebo in complex cardiovascular surgery: post hoc analysis and interpretation of phase III results. Interact Cardiovasc Thorac Surg. 2019;28:566–74.
Ranucci M, Baryshnikova E, Soro G, Ballotta A, De Benedetti D, Conti D. Multiple electrode whole-blood aggregometry and bleeding in cardiac surgery patients receiving thienopyridines. Ann Thorac Surg. 2011;91:123–129.
Ranucci M, Baryshnikova E, Crapelli GB, Rahe-Meyer N, Menicanti L, Frigiola A et al. Randomized, double-blinded, placebo-controlled trial of fibrinogen concentrate supplementation after complex cardiac surgery. J Am Heart Assoc. 2015;4:e002066.
Ranucci M, Pistuddi V, Baryshnikova E, Colella D, Bianchi P. Fibrinogen levels after cardiac surgical procedures: Association with postoperative bleeding, trigger values, and target values. Ann Thorac Surg. 2016;102:78–85.
Rourke C, Curry N, Khan S, Taylor R, Raza I, Davenport R et al. Fibrinogen levels during trauma hemorrhage, response to replacement therapy, and association with patient outcomes. J Thromb Haemost. 2012;10:1342–51.
Roy A, Sargent N, Rangarajan S, Alves S, Bell J, Stanford S et al. Fibrinogen concentrate vs cryoprecipitate in pseudomyxoma peritonei surgery: interim results from a prospective, randomized, controlled phase 2 study. Blood. 2018;132:2549.
Roy A, Stanford S, Nunn S, Alves S, Sargant N, Rangarajan S et al. Efficacy of fibrinogen concentrate in major abdominal surgery – A prospective, randomized, controlled study in cytoreductive surgery for pseudomyxoma peritonei. J Thromb Haemost. 2020;18:352–363.
Sabate A, Gutierrez R, Beltran J, Mellado P, Blasi A, Acosta F et al. Impact of preemptive fibrinogen concentrate on transfusion requirements in liver transplantation: A multicenter, randomized, double-blind, placebo-controlled trial. Am J Transplant. 2016;16:2421–9.
Sahin AS, Ozkan S. Treatment of obstetric hemorrhage with fibrinogen concentrate. Med Sci Monit. 2019;25:1814–21.
Schlimp CJ, Ponschab M, Voelckel W, Treichl B, Maegele M, Schöchl H. Fibrinogen levels in trauma patients during the first seven days after fibrinogen concentrate therapy: a retrospective study. Scand J Trauma Resusc Emerg Med. 2016;24:29.
Schöchl H, Nienaber U, Maegele M, Hochleitner G, Primavesi F, Steitz B et al. Transfusion in trauma: thromboelastometry-guided coagulation factor concentrate-based therapy versus standard fresh frozen plasma-based therapy. Crit Care. 2011;15:R83.
Seto S, Itakura A, Okagaki R, Suzuki M, Ishihara O. An algorithm for the management of coagulopathy from postpartum hemorrhage, using fibrinogen concentrate as first-line therapy. Int J Obstet Anaesth. 2017;32:11–16.
Simon L, Santi TM, Sacquin P, Hamza J. Pre-anaesthetic assessment of coagulation abnormalities in obstetric patients: usefulness, timing and clinical implications. Br J Anaesth. 1997;78:678–83.
Soleimani M, Masoumi N, Nooraei N, Lashay A, Safarinejad MR. The effect of fibrinogen concentrate on perioperative bleeding in transurethral resection of the prostate: a double-blind placebo-controlled and randomized study. J Thromb Haemost. 2017;15:255–62.
Solomon C, Pichlmaier U, Schoechl H, Hagl C, Raymondos K, Scheinichen D et al. Recovery of fibrinogen after administration of fibrinogen concentrate to patients with severe bleeding after cardiopulmonary bypass surgery. Br J Anaesth. 2010;104:555–62.
Solomon C, Cadamuro J, Ziegler B, Schöchl H, Varvenne M, Sørensen B et al. A comparison of fibrinogen measurement methods with fibrin clot elasticity assessed by thromboelastometry, before and after administration of fibrinogen concentrate in cardiac surgery patients. Transfusions. 2011;51:1695–796.
Solomon C, Schöchl H, Hanke A, Calatzis A, Hagl C, Tanaka K et al. Haemostatic therapy in coronary artery bypass graft patients with decreased platelet function: comparison of fibrinogen concentrate with allogeneic blood products. Scand J Clin Lab Invest. 2012;72:121–8.Sørensen B, Bevan D. A critical evaluation of cryoprecipitate for replacement of fibrinogen. British journal of haematology. 2010;149:834–43.
Spahn DR, Bouillon B, Cerny V, Duranteau J, Filipescu D, Hunt BJ et al. The European guideline on management of major bleeding and coagulopathy following trauma: fifth edition. Crit Care. 2019;23:98.
Stanworth SJ, Tinmouth AT. Plasma transfusion and use of albumin. In: Simon TL, editor. Rossi's Principles of Transfusion Medicine. 4th ed. Oxford, West Sussex, New Jersey: Blackwell Publishing; 2009:287–97.
Thachil J, Falanga A, Levi M, Liebman H, Di Nisio M, Scientific and Standardization Committee of the International Society on Thrombosis and Hemostasis. Management of cancer-associated disseminated intravascular coagulation: guidance from the SSC of the ISTH. J Thromb Haemost. 2015;13:671–5.
Theusinger OM, Baulig W, Seifert B, Emmert MY, Spahn DR, Asmis LM. Relative concentrations of haemostatic factors and cytokines in solvent/detergent‐treated and fresh‐frozen plasma. Br J Anaesth. 2011;106:505–11.
Tirotta CF, Lagueruela RG, Salyakina D, Wang W, Taylor T, Ojito J et al. Interval changes in ROTEM values during cardiopulmonary bypass in pediatric cardiac surgery patients. J Cardiothorac Surg. 2019;14.doi:10.1186/s13019-019-0949-0.
Wada H, Thachil J, Di Nisio M, Mathew P, Kurosawa S, Gando S et al. Guidance for diagnosis and treatment of DIC from harmonization of the recommendations from three guidelines. J Thromb Haemost. 2013;11:doi: 10.1111/jth.12155.
Wafaisade A, Lefering R, Maegele M, Brockamp T, Mutschler M, Lendemans S et al. Administration of fibrinogen concentrate in exsanguinating trauma patients is associated with improved survival at 6 hours but not at discharge. J Trauma Acute Care Surg. 2013;74:387–3.
Waldén K, Jeppsson A, Nasic S, Karlsson M. Fibrinogen concentrate to cardiac surgery patients with ongoing bleeding does not increase the risk of thromboembolic complications or death. Thromb Haemost. 2020;doi:10.1055/s-0039-3402759.
Wikkelsø AJ, Edwards HM, Afshari A, Stensballe J, Langhoff-Ross J, Albrechtsen C et al. Pre-emptive treatment with fibrinogen concentrate for postpartum haemorrhage: randomized controlled trial. Br J Anaesth. 2015;114:623–33.
Wong H, Curry N. Do we need cryoprecipitate in the era of fibrinogen concentrate and other specific factor replacement options? VOXS. 2018;13:23–28.
World Health Organization. Available at: http://whqlibdoc.who.int/publications/2010/9789241599375_eng.pdf (accessed 13 August 2019)
Yamamoto K, Usui A, Takamatsu J. Fibrinogen concentrate administration attributes to significant reductions of blood loss and transfusion requirements in thoracic aneurysm repair. Journal of Cardiothoracic Surgery. 2014;9:90.
Zadeh FJ, Janatmakan F, Soltanzadeh M, Zamankhani M. Investigating the effect of fibrinogen injection on bleeding in coronary artery bypass surgery: A clinical trial. Anesthesiol Pain Med. 2019;9:doi:10.5812/aapm.92165.
of interest
are looking at
saved
next event
Developed by EPG Health for Medthority in collaboration with CSL Behring, with content provided by CSL Behring.
Not intended for Healthcare Professionals outside Europe.

