Advances in diagnosis and management
Please answer this quick quiz before you read on. This helps us improve the educational design of our resources.
Pathways to clear diagnosis
Risk stratification for NMIBC
Non-muscle-invasive bladder cancer (NMIBC) is a clinically heterogeneous disease that has a high recurrence rate. Patients with high-risk NMIBC have elevated disease progression rates and represent approximately 25% of NMIBC cases.1,2
Patients with high-grade T1 bladder cancer have a 42% rate of 5-year recurrence, and a 21% progression rate3
Risk stratification of patients with NMIBC is crucial to ensure they receive appropriate treatments and surveillance schedules. Patients with high-risk NMIBC require a more intensive management and follow-up plan compared with those with low or intermediate risk.3,4
Figure 1 shows the risk stratification criteria according to the European Association of Urology (EAU) and the American Urological Association (AUA) and Society of Urologic Oncology (SUO). The National Comprehensive Cancer Network (NCCN) guidelines use the AUA/SUO criteria.5 Patients are stratified according to the number of tumors, tumor size, recurrence rate, tumor stage, presence of carcinoma in situ, and tumor grade, and are designated as low risk, intermediate risk, high risk, and very high risk.3
Figure 1. Risk stratification of NMIBC according to EAU and AUA/SUO.4,6 BCG, Bacillus Calmette–Guérin; CIS, carcinoma in situ; G1/2/3, grade 1/2/3; HG, high grade; LG, low grade; LVI, lymphovascular invasion.
High recurrence and progression rates demonstrate the need to accurately diagnose NMIBC and manage high-risk disease effectively to prevent progression.
Join Ashish Kamat and Félix Guerrero-Ramos in our podcast episode examining guideline-based approaches to NMIBC risk stratification.
Clinical presentation and differential diagnosis of NMIBC
Bladder cancer can coexist with, and mimic the symptoms of, urinary tract infections (UTIs), with 39% of women with bladder cancer initially misdiagnosed with UTIs, causing delays in treatment initiation3,7
Most cases of bladder cancer are diagnosed because of painless gross or microscopic hematuria.3,6 Gross hematuria (as opposed to microscopic hematuria) is associated with high-grade cancer, as statistically supported by a 2023 cross-sectional retrospective study (N=515).8
Around 20% of patients with NMIBC may present with increased urinary urgency, frequency, and dysuria.8 These features are more frequently observed in patients with carcinoma in situ than with papillary Ta/T1 tumors.3,9
Hear expert insights on NMIBC diagnosis with Ashish Kamat and Morgan Rouprêt and listen to a patient perspective on the journey before and after diagnosis in our podcast series.
Assessment of suspected bladder cancer
The precise diagnostic pathway for patients with NMIBC varies and should be individualized based on the patient’s risk of progression, and is dependent on resource availability.5,10
The initial evaluation of patients with suspected bladder cancers includes:3,5
- Focused patient history and physical examination
- Imaging of the abdomen/pelvis
- Cystoscopy
- Urinary cytology and biomarkers
- Histopathologic assessment
Of these, cystoscopy is still the universally recommended primary diagnostic tool and gold standard for the initial evaluation of patients with suspected bladder cancer.3
If a lesion is documented, transurethral resection of the bladder tumor (TURBT) should be carried out to confirm the diagnosis (and as part of initial surgical treatment).5 Figure 2 shows the diagnostic pathway, with the diagnostic tools discussed in detail below.
Figure 2. Diagnostic pathway for adults with suspected bladder cancer.3,5 CIS, carcinoma in situ; EUA, examination under anesthesia; MIBC, muscle-invasive bladder cancer; NCCN, National Comprehensive Cancer Network; NMIBC, non-muscle-invasive bladder cancer; TURBT, transurethral resection of bladder tumor.
Patient history and physical examination
EAU guidelines mandate a focused patient history and physical examination (although this will not reveal NMIBC).9 Considering 50% of bladder cancer cases are attributed to smoking, NCCN guidelines detail screening for smoking.5,11
Imaging of the abdomen/pelvis
According to the AUA/SUO guidelines, upper urinary tract imaging should be performed as part of the initial evaluation of patients with suspected bladder cancer, with computed tomography (CT) or magnetic resonance imaging (MRI) recommended.6 This is echoed by the NCCN guidelines, and imaging is recommended in parallel with cystoscopy (or in parallel with TURBT if not done prior to TURBT).5
By contrast, EAU guidelines recommend ultrasound and/or CT intravenous urography (IVU) during the initial evaluation and a CT urography only after a high-risk bladder tumor has been detected.9 CT urography can detect papillary tumors in the urinary tract, with IVU as an alternative if CT is not available.9
Ultrasound may be performed as an adjunct to physical examination since it can visualize intraluminal masses in the bladder, renal masses, and hydronephrosis, but it cannot exclude all causes of hematuria.9
Listen to our Managing High-Risk NMIBC podcast with Ashish Kamat and Morgan Rouprêt for expert insights on navigating multiple NMIBC guidelines – including imaging recommendations.
Cystoscopy
Cystoscopic examination and histologic evaluation of sampled tissue are necessary for the diagnosis of bladder cancer, with cystoscopy typically performed using white light (WL).9 All the most recent recommendations advise use of “enhanced cystoscopy,” namely photodynamic diagnosis (PDD; fluorescence cystoscopy or blue light cystoscopy) or narrow-band imaging (NBI), if the equipment is available.5,9,10
These new cystoscopic technologies have a demonstrably higher sensitivity than WL cystoscopy for detecting tumors, particularly high-risk tumors such as carcinoma in situ, but have lower specificity and cannot help to rule out prostatic involvement.3,12,13 PDD and NBI can be performed with flexible endoscopic equipment in the office.3,14
Urinary cytology and biomarkers
Urinary cytology can be performed as an adjunct to cystoscopy and has high sensitivity in detecting high-risk tumors, including carcinoma in situ.3,9 European guidelines advise analysis of voided urine (fresh urine or urine with adequate fixation), using the Paris System (2nd edition).9
Currently, EAU and AUA/SUO guidelines do not recommend any urinary biomarkers as part of routine clinical practice for diagnosis or follow-up.9,10 Other guidelines, such as the UK’s National Institute for Health and Care Excellence (NICE), recommend a urinary biomarker test (such as UroVysion using fluorescence in situ hybridization [FISH], ImmunoCyt, or a nuclear matrix protein 22 [NMP22] test) for patients with suspected bladder cancer.15
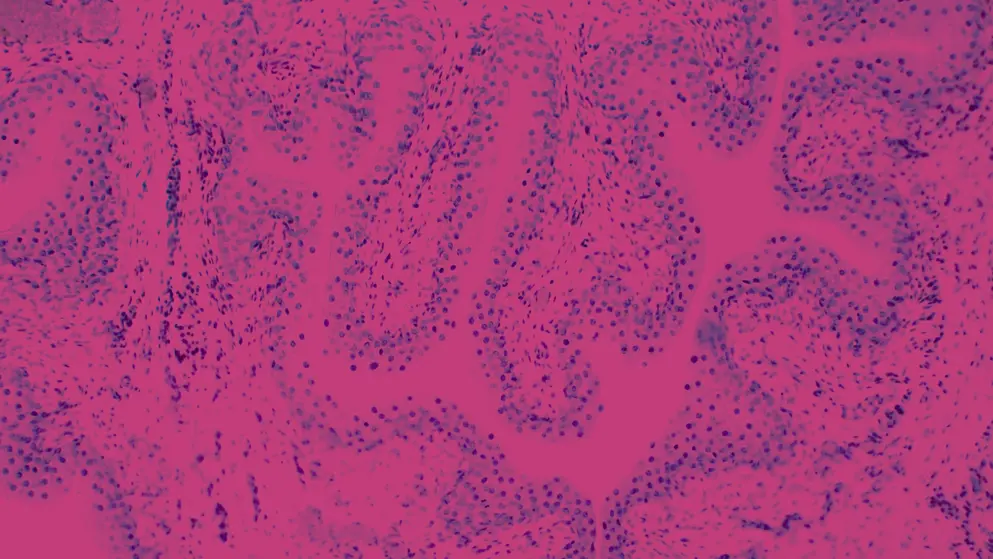
Histopathologic assessment
Histopathology of the tissue obtained through cystoscopy-guided biopsies and TURBT is one of the most reliable tools for assessing the depth of tumor infiltration, and hence essential for risk stratification of NMIBC.3
Of note, there is significant variability among pathologists regarding the diagnosis of carcinoma in situ, and there is inter-observer variability in the classification of stage T1 versus Ta tumors and tumor grading using both the 1973 and 2022 World Health Organization (WHO) classification.9
European guidelines strongly recommend using the 2017 TNM system to classify the depth of tumor invasion, and weakly recommend the use of both the 1973 and 2004/2022 WHO grading classification systems (or a hybrid system).9
TURBT
TURBT has key diagnostic and treatment roles – the goal is to confirm the clinical diagnosis and remove all visible lesions.3 A successful TURBT will identify the factors required to assign disease risk and clinical stage.9 To ensure accurate staging, guidelines recommend a second TURBT for certain patients, including those with incompletely resected tumors, T1 tumors, or with high-grade NMIBC, and a repeat TURBT is recommended 2–6 weeks after the initial TURBT.5,9,10
To ensure correct pathological assessment following TURBT, resected and analyzed tissue must be of high quality.9 EAU guidelines uniquely recommend use of a ‘TURBT checklist’ to support high-quality biopsy sample collection, shown in Figure 3.9
Figure 3. The TURBT checklist is recommended by EAU guidelines to obtain all relevant information for an accurate NMIBC diagnosis.9 CIS, carcinoma in situ; NBI, narrow-band imaging; NMIBC, non-muscle-invasive bladder cancer; PDD, photodynamic diagnosis; TURBT, transurethral resection of bladder tumor.
References
- Bedke, 2023. Optimizing outcomes for high-risk, non-muscle-invasive bladder cancer: The evolving role of PD-(L)1 inhibition. https://www.doi.org/10.1016/j.urolonc.2023.10.004
- Grabe-Heyne, 2023. Intermediate and high-risk non-muscle-invasive bladder cancer: An overview of epidemiology, burden, and unmet needs. https://www.doi.org/10.3389/fonc.2023.1170124
- Lopez-Beltran, 2024. Advances in diagnosis and treatment of bladder cancer. https://www.doi.org/10.1136/bmj-2023-076743
- Sylvester, 2021. European Association of Urology (EAU) prognostic factor risk groups for non–muscle-invasive bladder cancer (NMIBC) incorporating the WHO 2004/2016 and WHO 1973 classification systems for grade: An update from the EAU NMIBC Guidelines Panel. https://www.doi.org/10.1016/j.eururo.2020.12.033
- NCCN, 2024. NCCN clinical practice guidelines in oncology. Bladder cancer. Version 6.2024. https://www.nccn.org/professionals/physician_gls/pdf/bladder.pdf
- Chang, 2016. Diagnosis and treatment of non-muscle invasive bladder cancer: AUA/SUO guideline. https://www.doi.org/10.1016/j.juro.2016.06.049
- More than half of people with bladder cancer are misdiagnosed with another disease, 2023. https://worldbladdercancer.org/news_events/press-release-more-than-half-of-people-with-bladder-cancer-are-misdiagnosed-with-another-disease/
- Jakus, 2023. The impact of the initial clinical presentation of bladder cancer on histopathological and morphological tumor characteristics. https://www.doi.org/10.3390/jcm12134259
- Gontero, 2024. European Association of Urology guidelines on mon-muscle-invasive bladder cancer (TaT1 and carcinoma in situ)—A summary of the 2024 guidelines update. https://www.doi.org/10.1016/j.eururo.2024.07.027
- Holzbeierlein, 2024. Diagnosis and treatment of non-muscle invasive bladder cancer: AUA/SUO guideline: 2024 amendment. https://www.doi.org/10.1097/ju.0000000000003846
- Jubber, 2023. Epidemiology of bladder cancer in 2023: A systematic review of risk factors. https://www.doi.org/10.1016/j.eururo.2023.03.029
- Mowatt, 2011. Photodynamic diagnosis of bladder cancer compared with white light cystoscopy: Systematic review and meta-analysis. https://www.doi.org/10.1017/s0266462310001364
- Russo, 2021. Performance of narrow-band imaging (NBI) and photodynamic diagnosis (PDD) fluorescence imaging compared to white light cystoscopy (WLC) in detecting non-muscle invasive bladder cancer: A systematic review and lesion-level diagnostic meta-analysis. https://www.doi.org/10.3390/cancers13174378
- Wojcik, 2022. The Paris System for reporting urinary cytology. https://www.doi.org/10.1007/978-3-030-88686-8
- NICE, 2015. Bladder cancer: Diagnosis and management (NG2). https://www.nice.org.uk/guidance/ng2
The NMIBC treatment landscape
For patients with non-muscle-invasive bladder cancer (NMIBC), transurethral resection of the bladder tumor (TURBT) represents the mainstay in confirming diagnosis and risk stratification, as well as the initial treatment step.1,2 Where possible, the goal is to achieve complete resection of the tumor with the first (or repeat) TURBT.
The gold standard for post-TURBT treatment is intravesical instillation of Bacillus Calmette–Guérin (BCG); unfortunately, it has an estimated treatment failure rate of 40–50%.1 Treatment options for BCG-unresponsive disease have traditionally been scarce but, more recently, the treatment landscape began evolving (Figure 1).1
Figure 1. Initial management options for patients with low-, intermediate-, and high-risk NMIBC following risk stratification and TURBT with or without intravesical chemotherapy.3-6 Nadofaragene firadenovec-vncg and nogapendekin alfa inbakicept (NAI) are only approved for use in the USA.5,6 AUA, American Urology Association; BCG, Bacillus Calmette–Guérin.
Unmet needs in NMIBC
NMIBC can be challenging to manage, with significant rates of treatment failure and disease progression, especially for high-risk patients.7
Despite BCG treatment, around 20% of patients with high-risk NMIBC progress to muscle-invasive disease8
For patients with BCG-unresponsive disease or with “very high-risk” features, radical cystectomy remains the preferred recommended option.1,3,9-11 While potentially curative, patients undergoing radial cystectomy experience considerable physical and psychological burdens, as well as urinary and sexual dysfunction, which may significantly impact quality of life.1,7
Far more radical cystectomies are canceled due to patient lack of consent than medical contraindications.1 Reflecting this, results from a qualitative study show that patient respondents (N=107) were willing to accept a 44% increase in the risk of progression to MIBC, in order to delay radical cystectomy for 5 years.12 The considerable hesitation toward radical cystectomy shown by patients highlights a need for expanded bladder-sparing treatment approaches.
Intravesical BCG for high-risk NMIBC
The precise mechanism of action of intravesical BCG remains to be defined; however, it is known to trigger innate and adaptive immune responses leading to the destruction of cancerous cells.13
While a first-line therapy, BCG has many adverse events that can impact treatment adherence; in a European study, around 70% of patients (N=1,316) experienced local or systemic adverse events and 8% discontinued due to toxicity.14
Potential adverse events and toxicities of BCG include:
- Urinary frequency14
- Cystitis14
- Fever14
- Hematuria14
- Granulomatous prostatitis15,16
- Epididymo-orchitis17
- Distant infections, such as granulomatous pneumonia, hepatitis, aortic infection, dermatologic and ophthalmic manifestations and, more rarely, sepsis13
Unfortunately, global shortage of BCG continues to be an issue despite efforts to increase its production.18,19 The European Association of Urology (EAU) and American Urology Association (AUA) prioritize full-strength BCG for patients with high-risk NMIBC.19,20 If BCG is unavailable, intravesical chemotherapy or radical cystectomy are alternative options; however, treatment with the former is associated with a higher risk of recurrence compared with BCG immunotherapy.20
The global shortage of BCG, in addition to its potential adverse events and the high proportion of patients with BCG-unresponsive disease, has driven the development of alternative immunotherapies for patients with high-risk NMIBC.18
PD1/PD-L1 inhibition
Pembrolizumab was approved for NMIBC in 2020 and was the first alternative option to radical cystectomy for patients with BCG-unresponsive disease.4,13,21,22 While BCG is a nonspecific and intravesical immunotherapy, pembrolizumab is an intravenously administered monoclonal immunoglobulin (Ig)G4 antibody, specifically inhibiting the immune checkpoint protein programmed cell death 1 (PD-1).1
Systemic pembrolizumab was approved following data from the KEYNOTE-057 study, in which 41% of participants (N=101) with BCG-unresponsive NMIBC receiving 200 mg pembrolizumab every 3 weeks had a complete response at 3 months, 46% of whom maintained a response for at least 12 months.23,24 Regarding safety, 13% of participants experienced grade 3 or 4 treatment-related adverse events, and 22% had immune-related adverse events.23
In a recent KEYNOTE-057 analysis, 43.5% of participants with BCG-unresponsive high-grade Ta or any-grade T1 tumors without carcinoma in situ (CIS; N=132) had 12-month disease-free survival (DFS).24
The 2024 AUA / Society of Urologic Oncology (SUO) Guideline amendment recommends offering pembrolizumab to patients with CIS completing adequate BCG therapy within 12 months.11 The 2024 National Comprehensive Cancer Network (NCCN) guidelines recommend pembrolizumab for the treatment of patients with BCG-unresponsive, high-risk disease with either CIS or high-grade papillary Ta/T1-only tumors who are ineligible for or have elected not to undergo cystectomy.3
By contrast, European guidelines give a weak recommendation for systemic immunotherapy in BCG-unresponsive tumors, since all alternatives are considered inferior to radical cystectomy.10
Programmed death-ligand 1 (PD-L1) expression in tumors may play a role in attenuating responses to BCG; it has been speculated that by inhibiting PD-1 interaction with its ligands PD-L1 and PD-L2, pembrolizumab may improve the antitumor activity of BCG. The efficacy and safety of pembrolizumab in combination with BCG in BCG-naive patients with high-risk NMIBC is being investigated in KEYNOTE-676, an open-label, comparator-controlled phase 3 study currently underway.25
IL-15 agonism
Interleukin 15 (IL-15) is a potent stimulator of CD8+ T cells, memory T cells, and natural killer cells, all of which can reduce the tumor burden.5 IL-15 superagonist nogapendekin alfa inbakicept-pmin (NAI) received U.S. Food and Drug Administration (FDA) approval for NMIBC in April 2024; it is currently only approved in the USA for use in combination with BCG in patients with BCG-unresponsive NMIBC CIS with or without papillary tumors.5,26
NAI is administered intravesically with BCG as induction therapy once a week for 6 weeks, with a second induction course administered if complete response is not achieved at month 3, followed by maintenance therapy. Maintenance therapy consists of NAI administration with BCG once a week for 3 weeks at months 4, 7, 10, 13, and 19 for a total of 15 doses.5
The approval for NAI came following data from the ongoing QUILT-3.032 trial: in a cohort of patients with BCG-unresponsive CIS treated with NAI combined with BCG, complete response at any time was achieved in 71% of participants (N=82).27 For participants who experienced a complete response, the estimated probability of avoiding cystectomy at month 24 was 89.2% and disease-specific survival was estimated to be 100%. In participants with BCG-unresponsive high-grade Ta/T1 papillary NMIBC (N=72), the estimated DFS was 55.4% at 12 months.27
Most treatment-emergent adverse events with NAI plus BCG were grade 1 or 2 and were experienced by 86% of participants; three grade 3 immune-related adverse events occurred.27
The most recent NCCN guidelines (October 2024) recommend NAI plus BCG as an option for BCG-unresponsive/BCG-intolerant patients with high-risk NMIBC CIS.3 The recent International Bladder Cancer Group Recommendations (August 2024) also recommend (off-label) considering NAI plus BCG for patients with BCG-unresponsive, high-grade papillary Ta/T1 tumors without CIS, and BCG-unresponsive papillary-only tumors.4
Applications for regulatory approval of NAI in the European Union and UK have been submitted and are currently pending.28,29 Furthermore, trials to investigate the efficacy and safety of NAI in BCG-naive disease are planned (QUILT-2.005), with enrollment of patients in the USA, India, and South Africa scheduled.29
Other immunotherapies
Additional immunotherapies are currently under investigation for the treatment of patients with NMIBC, including:1
- Atezolizumab (PD-L1 inhibitor)
- Durvalumab (PD-L1 inhibitor)
- Nivolumab (PD-1 inhibitor)
- Sasanlimab (PD-1 inhibitor)
References
- Jaromin, 2024. Revolutionizing treatment: Breakthrough approaches for BCG-unresponsive non-muscle-invasive bladder cancer. https://www.doi.org/10.3390/cancers16071366
- Babjuk, 2022. European Association of Urology guidelines on non–muscle-invasive bladder cancer (Ta, T1, and carcinoma in situ). https://www.doi.org/10.1016/j.eururo.2021.08.010
- NCCN, 2024. NCCN clinical practice guidelines in oncology. Bladder cancer. Version 6.2024. https://www.nccn.org/professionals/physician_gls/pdf/bladder.pdf
- Li, 2024. Bladder-sparing therapy for Bacillus Calmette-Guérin–unresponsive non–muscle-invasive bladder cancer: International Bladder Cancer Group recommendations for optimal sequencing and patient selection. https://www.doi.org/10.1016/j.eururo.2024.08.001
- Keam, 2024. Nogapendekin alfa inbakicept: First approval. https://www.doi.org/10.1007/s40265-024-02060-1
- Lee, 2023. Nadofaragene firadenovec: First approval. https://www.doi.org/10.1007/s40265-023-01846-z
- Grabe-Heyne, 2023. Intermediate and high-risk non-muscle-invasive bladder cancer: An overview of epidemiology, burden, and unmet needs. https://www.doi.org/10.3389/fonc.2023.1170124
- Van Den Bosch, 2011. Long-term cancer-specific survival in patients with high-risk, non–muscle-invasive bladder cancer and tumour progression: A systematic review. https://www.doi.org/10.1016/j.eururo.2011.05.045
- NICE, 2015. Bladder cancer: Diagnosis and management (NG2). https://www.nice.org.uk/guidance/ng2
- Gontero, 2024. European Association of Urology guidelines on mon-muscle-invasive bladder cancer (TaT1 and carcinoma in situ)—A summary of the 2024 guidelines update. https://www.doi.org/10.1016/j.eururo.2024.07.027
- Holzbeierlein, 2024. Diagnosis and treatment of non-muscle invasive bladder cancer: AUA/SUO guideline: 2024 amendment. https://www.doi.org/10.1097/ju.0000000000003846
- Collacott, 2023. Patient preferences for treatment of Bacillus Calmette-Guérin–unresponsive non–muscle-invasive bladder cancer: A cross-country choice experiment. https://www.doi.org/10.1016/j.euros.2022.12.016
- Lidagoster, 2024. BCG and alternative therapies to BCG therapy for non-muscle-invasive bladder cancer. https://www.doi.org/10.3390/curroncol31020079
- Brausi, 2014. Side effects of Bacillus Calmette-Guérin (BCG) in the treatment of intermediate- and high-risk Ta, T1 papillary carcinoma of the bladder: Results of the EORTC Genito-Urinary Cancers Group randomised phase 3 study comparing one-third dose with full dose and 1 year with 3 years of maintenance BCG. https://www.doi.org/10.1016/j.eururo.2013.07.021
- Oates, 1988. Granulomatous prostatitis following Bacillus Calmette-Guerin immunotherapy of bladder cancer. https://www.doi.org/10.1016/s0022-5347(17)41803-9
- Logan, 2014. Changes observed in multiparametric prostate magnetic resonance imaging characteristics correlate with histopathological development of chronic granulomatous prostatitis after intravesical Bacillus Calmette-Guerin therapy. https://www.doi.org/10.1097/rct.0b013e3182aac58a
- Harada, 2006. Epididymo‐orchitis caused by intravesically instillated bacillus Calmette‐Guérin: Genetically proven using a multiplex polymerase chain reaction method. https://www.doi.org/10.1111/j.1442-2042.2006.01257.x
- Passarelli, 2024. Contemporary treatment of NMIBC—Is it time to move on from BCG? https://www.doi.org/10.3390/jcm13144112
- American Urological Association, 2020. BCG shortage info: October 2020 announcement about BCG production, supply. https://www.auanet.org/about-us/bcg-shortage-info
- Babjuk, 2012. Statement concerning the shortage of BCG vaccine from the EAU Guidelines Panel on non-muscle invasive bladder cancer. https://d56bochluxqnz.cloudfront.net/documents/guideline-publications/non-muscle-invasive-bladder-cancer/NMIBC-Guidelines-Panel-Statement-Concerning-Shortage-of-BCG-Vaccine.pdf
- Keytruda PI, 2025. https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/125514s172lbl.pdf
- Keytruda SPC, 2025. https://www.ema.europa.eu/en/documents/product-information/keytruda-epar-product-information_en.pdf
- Balar, 2021. Pembrolizumab monotherapy for the treatment of high-risk non-muscle-invasive bladder cancer unresponsive to BCG (KEYNOTE-057): An open-label, single-arm, multicentre, phase 2 study. https://www.doi.org/10.1016/s1470-2045(21)00147-9
- Necchi, 2024. Pembrolizumab monotherapy for high-risk non-muscle-invasive bladder cancer without carcinoma in situ and unresponsive to BCG (KEYNOTE-057): A single-arm, multicentre, phase 2 trial. https://www.doi.org/10.1016/s1470-2045(24)00178-5
- UroToday, 2024. ASCO GU 2024: Phase 3 KEYNOTE-676 cohort A: Bacillus Calmette-Guérin with or without pembrolizumab for high-risk non–muscle-invasive bladder cancer that persists/recurs after BCG induction. https://www.urotoday.com/conference-highlights/asco-gu-2024/asco-gu-2024-bladder-cancer/149535-asco-gu-2024-phase-3-keynote-676-cohort-a-bacillus-calmette-guerin-with-or-without-pembrolizumab-for-high-risk-non-muscle-invasive-bladder-cancer-that-persists-recurs-after-bcg-induction.html
- Anktiva PI, 2024. https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/761336s000lbl.pdf
- Chamie, 2023. IL-15 superagonist NAI in BCG-unresponsive non–muscle-invasive bladder cancer. https://www.doi.org/10.1056/evidoa2200167
- OncLive, 2024. Nogapendekin alfa inbakicept plus BCG maintains CR rate in BCG-unresponsive NMIBC with CIS. 19 November. https://www.onclive.com/view/nogapendekin-alfa-inbakicept-plus-bcg-maintains-cr-rates-in-bcg-unresponsive-nmibc-with-cis
- ImmunityBio’s ANKTIVA® now covered by more than a dozen insurance plans representing over 100 million lives within months of FDA approval, 2024. https://ir.immunitybio.com/news-releases/news-release-details/immunitybios-anktivar-now-covered-more-dozen-insurance-plans
The evolving treatment landscape
Transurethral resection of the bladder tumor (TURBT) is the preferred treatment for patients with non-muscle-invasive bladder cancer (NMIBC), with intravesical Bacillus Calmette–Guérin (BCG) therapy or radical cystectomy recommended for high-risk patients post-TURBT.1-3 Unfortunately, BCG therapy has an estimated treatment failure of 40–50%, and radical cystectomy significantly impacts quality of life.3 Hence, in recent years, efforts have focused on expanding treatment options for high-risk NMIBC.3
Since 2020, three treatments have been approved for patients in the USA with BCG-unresponsive, high-risk NMIBC with carcinoma in situ (CIS) with or without papillary tumors
In January 2020, the US Food and Drug Administration (FDA) approved pembrolizumab, the first anti-programmed cell death 1 (anti-PD-1) therapy for this indication.4,5 In the KEYNOTE-057 study, 41% of participants (N=101) receiving pembrolizumab had a complete response (CR) at 3 months, 46% of whom maintained a response for at least 12 months.6,7 However, 13% of participants experienced grade 3 or 4 treatment-related adverse events.6 Pembrolizumab is also approved in Australia but not in Europe.8,9
In December 2022, nadofaragene firadenovec (NFF) became the first intravesical gene therapy and interferon alpha therapy to receive FDA approval.10,11 In a phase 3 study, 53.4% of patients with CIS (n=103) showed a CR within 3 months of the first dose of NFF, and of those, 45.5% (n=55) maintained a CR at 12 months.12 The null hypothesis specified a CR rate of <27%.12 At the end of 5 years of follow-up, 85% of patients with CIS experienced recurrence of high-grade disease, though no new safety signals emerged.13
In April 2024, the interleukin-15 (IL-15) receptor agonist nogapendekin alfa inbakicept-pmln (NAI), in combination with BCG, was approved in the USA.14,15 In the QUILT-3.032 trial, 71% of patients (N=82) with BCG-unresponsive CIS achieved CR at any time.16 In patients with BCG-unresponsive high-grade Ta/T1 papillary NMIBC (n=72), the estimated disease-free survival was 55.4% at 12 months.16 Most treatment-emergent adverse events with NAI plus BCG were grade 1 or 2.16 Applications for regulatory approval of NAI in the European Union and UK have been submitted and are currently pending.17,18
Other treatments under investigation for NMIBC include:
- Additional PD-1/PD-ligand 1 (PD-L1) inhibitors
- Intravesical chemotherapy combinations
- Novel local delivery systems
- Viral and bacterial-based therapy
- Targeted therapies
Emerging immunotherapies
Sasanlimab
In January 2025, it was revealed that the phase 3 CREST trial with the subcutaneous anti-PD-1 monoclonal antibody sasanlimab met its primary endpoint.19
Sasanlimab, in combination with BCG, significantly improved event-free survival (EFS) in patients with BCG-naive high-risk NMIBC versus BCG therapy19
Sasanlimab (in combination with BCG) is the first PD-1 inhibitor to prolong EFS in this patient population, and its safety profile with BCG was generally consistent with prior reports of BCG, PD-1 inhibitors, and sasanlimab.19
Atezolizumab
Phase 1b/2 results with the intravenous PD-L1 inhibitor atezolizumab, in combination with BCG, demonstrated that 2-year high-grade recurrence-free survival was 83.2% in patients with high-risk NMIBC (N=36).20 No toxic deaths were reported. Atezolizumab in combination with BCG will be investigated in the phase 3 ALBAN study.20
Durvalumab
In 17 patients with BCG-unresponsive CIS-containing NMIBC, only 12% achieved CR with the intravenous formulation of PD-L1 inhibitor durvalumab at 6 months, and no patient had durable response at 24 months.21 In another phase 2 trial, 30 patients with BCG-unresponsive NMIBC were treated with the intravesical formulation of durvalumab; the high-grade relapse-free rate at 1 year was 39%, and the only adverse event was hematuria.22 Durvalumab in combination with BCG is being investigated in the phase 3 POTOMAC and PATAPSCO studies.23,24
Therapeutic combinations for NMIBC
Sequential intravesical chemotherapy with agents like gemcitabine/docetaxel is an increasingly studied alternative to radical cystectomy.1 In 75 patients with BCG-unresponsive high-risk and very-high-risk NMIBC treated with gemcitabine/docetaxel, the 1-year disease-free survival was 73%, while the 1-year progression-free survival (PFS) was 95%.25 Adverse events occurred in 45% of patients.25
Novel delivery systems
TAR-200
In December 2023, the FDA granted TAR-200 Breakthrough Therapy designation for the treatment of adults with BCG-unresponsive high-risk NMIBC with CIS who are ineligible for or decline radical cystectomy.26
Updated results from the phase 2b SunRISe-1 study showed an 84% CR rate at any time for patients with BCG-unresponsive high-risk NMIBC (n=85).27 No treatment-related deaths occurred, and 6% of patients discontinued treatment due to adverse events.27
In January 2025, a New Drug Application was submitted to the FDA for TAR-200: an investigational intravesical system that provides sustained local delivery of gemcitabine into the bladder for treating BCG-unresponsive high-risk NMIBC with CIS. In Europe, TAR-200 is accessible via clinical trials.26
Electromotive drug administration
Electromotive drug administration (EMDA) is an advanced approach to enhance the delivery of intravesical chemotherapy to the bladder wall.1
In a UK-based single-center study published in 2016, 107 patients with high-risk NMIBC were treated with sequential BCG/EMDA-mitomycin C (BCG/EMDA-MMC) post-TURBT.28 Following first-check cystoscopy, 87% of patients showed CR. At 1 and 2 years, respectively, 87% and 93% remained recurrence-free. Tolerability was “acceptable although challenging” due to adverse events; 28% of patients did not complete the full course of treatment, with half of those patients discontinuing due to adverse events including lower urinary tract symptoms and/or hematuria.28
In a small, retrospective study, PFS rates were 58.3% at 1 year and 48.9% at 2 years for patients with BCG-unresponsive NMIBC receiving BCG/EMDA-MMC (N=26).29 In this study, 15% of patients did not complete the full protocol, and 15.4% of patients died of bladder cancer.29
Viral and bacterial-based therapy
CG0070
Cretostimogene grenadenorepvec (CG0070) is an oncolytic adenovirus targeting bladder tumor cells with defective retinoblastoma-pathway gene expression.30
In the ongoing phase 3 BOND-003 trial, intravesical CG0070 monotherapy achieved a 74.5% CR rate at any time in patients with BCG-unresponsive high-risk NMIBC with CIS.31 Treatment was well tolerated with no grade ≥3 treatment-related adverse events, and 97.3% of patients completed treatment.31 In the phase 2 CORE-001 trial combining CG0070 with pembrolizumab, a CR rate of 92% at 3 months was observed in patients with BCG-unresponsive NMIBC (N=35).32
TARA-002
Results from the ongoing phase 2 ADVANCED-2 trial of TARA-002, an investigational cell-based therapy, in patients with high-risk NMIBC with CIS who were either BCG-naive or BCG-responsive (N=20), were announced in December 2024.33 The CR rate was 72% at 6 months, and 70% at any time. There were no grade ≥2 treatment-related adverse events, and no patients discontinued due to adverse events.33
Targeted therapy
Erdafitinib
Erdafitinib, the oral, selective pan-fibroblast growth factor receptor (pan-FGFR) inhibitor, is currently approved for locally advanced or metastatic urothelial cancer (UC) in patients with FGFR3 alterations.30 As these alterations are also associated with NMIBC, erdafitinib is being investigated in patients with BCG-unresponsive high-risk NMIBC with select FGFR2/3 alterations.34
In the phase 2 THOR-2 trial, erdafitinib had a clear benefit in comparison with chemotherapy in relation to relapse-free survival curves. Although there were no treatment-related deaths, 29% of participants discontinued erdafitinib due to treatment-related adverse events.35
Enfortumab vedotin
Enfortumab vedotin (EV) targets Nectin-4 and is an antibody–drug conjugate approved in combination with pembrolizumab for first-line treatment of adults with locally advanced or metastatic UC. EV in intravesical formulation for BCG-unresponsive NMIBC is being studied in a phase 1 trial.30
Please note, this is not an exhaustive list of all investigational treatments for high-risk NMIBC. For expert perspectives on emerging therapies, evolving standards of care, and future directions in high-risk NMIBC, listen to our podcast episode with Joshua Meeks and Ashish Kamat.
References
- Gontero, 2024. European Association of Urology guidelines on non–muscle-invasive bladder cancer (TaT1 and Carcinoma In Situ)—A summary of the 2024 guidelines update. https://www.doi.org/10.1016/j.eururo.2024.07.027
- Holzbeierlein, 2024. Diagnosis and treatment of non-muscle invasive bladder cancer: AUA/SUO guideline: 2024 amendment. https://www.doi.org/10.1097/ju.0000000000003846
- Jaromin, 2024. Revolutionizing treatment: Breakthrough approaches for BCG-unresponsive non-muscle-invasive bladder cancer. https://www.doi.org/10.3390/cancers16071366
- FDA approves Merck’s KEYTRUDA® (pembrolizumab) for patients with BCG-unresponsive, high-risk, non-muscle invasive bladder cancer with carcinoma in situ with or without papillary tumors who are ineligible for or have elected not to undergo cystectomy, 2020. https://www.merck.com/news/fda-approves-mercks-keytruda-pembrolizumab-for-patients-with-bcg-unresponsive-high-risk-non-muscle-invasive-bladder-cancer-with-carcinoma-in-situ-with-or-without-papillary-tumors-wh/
- Keytruda PI, 2025. https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/125514s172lbl.pdf
- Balar, 2021. Pembrolizumab monotherapy for the treatment of high-risk non-muscle-invasive bladder cancer unresponsive to BCG (KEYNOTE-057): An open-label, single-arm, multicentre, phase 2 study. https://www.doi.org/10.1016/s1470-2045(21)00147-9
- Necchi, 2024. Pembrolizumab monotherapy for high-risk non-muscle-invasive bladder cancer without carcinoma in situ and unresponsive to BCG (KEYNOTE-057): A single-arm, multicentre, phase 2 trial. https://www.doi.org/10.1016/s1470-2045(24)00178-5
- Keytruda Australian PI, 2023. https://www.tga.gov.au/sites/default/files/2023-06/auspar-keytruda-230609-pi.pdf
- Keytruda SPC, 2025. https://www.ema.europa.eu/en/documents/product-information/keytruda-epar-product-information_en.pdf
- Steinmetz, 2024. The evolution of nadofaragene firadenovec: A review and the path forward. https://www.doi.org/10.3233/blc-230083
- Adstiladrin PI, 2024. https://www.fda.gov/media/164029/download
- Boorjian, 2021. Intravesical nadofaragene firadenovec gene therapy for BCG-unresponsive non-muscle-invasive bladder cancer: a single-arm, open-label, repeat-dose clinical trial. https://www.doi.org/10.1016/S1470-2045(20)30540-4
- Narayan, 2024. Efficacy of intravesical nadofaragene firadenovec for patients with Bacillus Calmette-Guerin-unresponsive non-muscle-invasive bladder cancer: 5-year follow-up from a phase 3 trial. https://www.doi.org/10.1097/JU.0000000000004020
- Anktiva PI, 2024. https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/761336s000lbl.pdf
- Keam, 2024. Nogapendekin alfa inbakicept: First approval. https://www.doi.org/10.1007/s40265-024-02060-1
- Chamie, 2023. IL-15 superagonist NAI in BCG-unresponsive non–muscle-invasive bladder cancer. https://www.doi.org/10.1056/evidoa2200167
- OncLive. 2024. Nogapendekin alfa inbakicept plus BCG maintains CR rate in BCG-unresponsive NMIBC with CIS. 19 November. https://www.onclive.com/view/nogapendekin-alfa-inbakicept-plus-bcg-maintains-cr-rates-in-bcg-unresponsive-nmibc-with-cis
- ImmunityBio’s ANKTIVA® now covered by more than a dozen insurance plans representing over 100 million lives within months of FDA approval, 2024. https://ir.immunitybio.com/news-releases/news-release-details/immunitybios-anktivar-now-covered-more-dozen-insurance-plans
- Pfizer. 2024. Press release: Pfizer’s sasanlimab in combination with BCG improves event-free survival in patients with BCG-naïve, high-risk non-muscle invasive bladder cancer. https://www.pfizer.com/news/press-release/press-release-detail/pfizers-sasanlimab-combination-bcg-improves-event-free
- UroToday, 2024. EAU 2024: First results of the phase Ib-II BladderGATE clinical trial: Intravenous atezolizumab + intravesical Bacillus Calmette-Guérin (BCG) upfront combination in BCG-naïve high risk non-muscle invasive bladder cancer patients. https://www.urotoday.com/conference-highlights/eau-2024/eau-2024-bladder-cancer/151012-eau-2024-first-results-of-the-phase-ib-ii-bladdergate-clinical-trial-intravenous-atezolizumab-intravesical-bacillus-calmette-guerin-bcg-upfront-combination-in-bcg-naive-high-risk-non-muscle-invasive-bladder-cancer-patients.html
- Li, 2023. A phase II study of durvalumab for Bacillus Calmette-Guerin (BCG) unresponsive urothelial carcinoma in situ of the bladder. https://www.doi.org/10.1158/1078-0432.CCR-23-0354
- Fragkoulis, 2025. Intravesical administration of durvalumab for high-risk non-muscle-invasive bladder cancer: A phase 2 study by the Hellenic GU Cancer Group. https://www.doi.org/10.1016/j.eururo.2024.12.018
- NCT05943106, 2025. BCG in combination with durvalumab in adult BCG-naïve, high-risk NMIBC participants (PATAPSCO). https://clinicaltrials.gov/study/NCT05943106
- NCT03528694, 2024. Assessment of efficacy and safety of durvalumab plus BCG compared to the standard therapy with BCG in non-muscle invasive bladder cancer (POTOMAC). https://clinicaltrials.gov/study/NCT03528694
- Scilipoti, 2025. Gemcitabine and docetaxel for high‐risk non‐muscle‐invasive bladder cancer: EuroGemDoce group results. https://www.doi.org/10.1111/bju.16645
- New Drug Application initiated with U.S. FDA for TAR-200, the first and only intravesical drug releasing system for patients with BCG-unresponsive high-risk non-muscle-invasive bladder cancer, 2025. https://www.jnj.com/media-center/press-releases/new-drug-application-initiated-with-u-s-fda-for-tar-200-the-first-and-only-intravesical-drug-releasing-system-for-patients-with-bcg-unresponsive-high-risk-non-muscle-invasive-bladder-cancer
- Van Der Heijden, 2024. LBA85 TAR-200 +/- cetrelimab (CET) and CET alone in patients (pts) with bacillus Calmette-Guérin-unresponsive (BCG UR) high-risk non-muscle-invasive bladder cancer (HR NMIBC): Updated results from SunRISe-1 (SR-1). https://www.doi.org/10.1016/j.annonc.2024.08.2329
- Gan, 2016. Sequential bacillus Calmette-Guérin/electromotive drug administration of mitomycin C as the standard intravesical regimen in high risk non-muscle invasive bladder cancer: 2-year outcomes. https://www.doi.org/10.1016/j.juro.2016.01.103
- Juvet, 2020. Sequential administration of Bacillus Calmette-Guerin (BCG) and electromotive drug administration (EMDA) of mitomycin C (MMC) for the treatment of high-grade nonmuscle invasive bladder cancer after BCG failure. https://www.doi.org/10.1016/j.urolonc.2020.06.031
- Li, 2024. Bladder-sparing therapy for Bacillus Calmette-Guérin–unresponsive non–muscle-invasive bladder cancer: International Bladder Cancer Group recommendations for optimal sequencing and patient selection. https://www.doi.org/10.1016/j.eururo.2024.08.001
- UroToday, 2024. SUO 2024: Topline results from BOND-003: A phase-3 study of intravesical cretostimogene grenadenorepvec for the treatment of high-risk BCG-unresponsive NMIBC with CIS. https://www.urotoday.com/conference-highlights/suo-2024/suo-2024-bladder-cancer/156717-suo-2024-topline-results-from-bond-003-a-phase-3-study-of-intravesical-cretostimogene-grenadenorepvec-for-the-treatment-of-high-risk-bcg-unresponsive-nmibc-with-cis.html
- Li, 2022. 666 Phase 2, single arm study of CG0070 combined with pembrolizumab in patients with non-muscle invasive bladder cancer (NMIBC) unresponsive to bacillus calmette-guerin (BCG). https://dx.doi.org/10.1136/jitc-2022-SITC2022.0666
- Protara announces positive results from the ongoing phase 2 ADVANCED-2 trial of TARA-002 in patients with NMIBC, 2024. https://ir.protaratx.com/news-releases/news-release-details/protara-announces-positive-results-ongoing-phase-2-advanced-2
- Drouaud, 2025. Novel immunotherapies and targeted molecular therapies for non-muscle invasive bladder cancer: a literature review. https://www.doi.org/10.21037/amj-23-222
- Catto, 2024. Erdafitinib in BCG-treated high-risk non-muscle-invasive bladder cancer. https://www.doi.org/10.1016/j.annonc.2023.09.3116
Selecting the best care pathway
When selecting the most appropriate therapy for patients with non-muscle-invasive bladder cancer (NMIBC), it is crucial to balance oncologic efficacy with tolerability and patient quality of life (QoL).1
Patients with Bacillus Calmette–Guérin (BCG)-unresponsive NMIBC must be informed that radical cystectomy is the recommended standard of care and provides the most durable disease control2
Unfortunately, radical cystectomy is associated with a substantial reduction in QoL.3 In particular, urinary and sexual dysfunction are persistently worse 2 years post-radical cystectomy compared with the general population.3 This option is not suitable for some patients due to age, comorbidities, or patient refusal to accept radical surgery.4
Considering the recent and ongoing increase in the number of bladder-sparing therapies (BST) available, patients who refuse, or are ineligible for, radical cystectomy should receive counseling on the efficacy, toxicity, and QoL parameters of each BST option2
Hear how patient priorities shape NMIBC treatment decisions in our podcast with Ashish Kamat, patient Doug Cappiello, and caregiver Camille Cappiello.
For practical strategies on tailoring first-line NMIBC treatment to individual patient needs, including supporting patients through BCG therapy and cystectomy, listen to our podcast with Kamat and Fred Witjes.
Recommended bladder-sparing therapies
The International Bladder Cancer Group (IBCG) recommends the following BSTs for BCG-unresponsive carcinoma in situ (CIS):2
- Gemcitabine/docetaxel (not specifically approved for this patient subgroup, but may be considered on the basis of available data)
- Nadofaragene firadenovec (NFF)
- Nogapendekin alfa inbakicept-pmln (NAI) plus BCG
- Pembrolizumab (to be considered only in patients who have exhausted more tolerable alternative options)
For patients with BCG-unresponsive papillary-only tumors, the IBCG recommends the following treatments (not all are specifically approved for this patient subgroup, but may be considered on the basis of available data):2
- Gemcitabine/docetaxel
- NFF
- Pembrolizumab
- NAI plus BCG
- Single-agent chemotherapy
- Hyperthermic mitomycin C
Selecting the optimal BST requires an individualized approach, with treatment tailored to tumor and patient characteristics, efficacy, QoL considerations, patient preferences, and real-world access to care.2
Improvements can still be made to current BST therapies, particularly with respect to durability of response, but there is an absence of randomized clinical trials (RCTs) for these options.2 Therefore, the IBCG recommends that patients with BCG-unresponsive NMIBC who refuse, or are ineligible for, radical cystectomy should be counseled to consider participating in a clinical trial. RCTs can also establish which combinations of therapies may have additive or synergistic efficacy.2
Addressing patient needs
Due to the invasive nature of treatment regimens and surveillance protocols, as well as QoL implications and physical symptoms associated with NMIBC, people living with the disease may require additional care to support their treatment journey.5
This may include support for psychological, physical, practical, interpersonal, family, social, and healthcare communications needs, as detailed in Figure 1.5
Figure 1. The varying needs of patients with NMIBC, which may persist throughout their diagnostic and treatment journey. NMIBC, non-muscle-invasive bladder cancer.5
Furthermore, recently approved and emerging therapies for the treatment of NMIBC, such as programmed cell death 1 (PD-1) inhibitors, require additional support for the monitoring and management of immune-related adverse events (AEs) from medical specialists beyond urologists and oncologists.6 Pembrolizumab, approved by the US Food and Drug Administration (FDA) for BCG-unresponsive high-risk NMIBC, is not commonly used due to its need for multidisciplinary monitoring for systemic toxicity.6
Benefits of cross-specialist support
Early intervention for immune-related AEs, such as respiratory, gastrointestinal, and rheumatology-related AEs, is crucial to ensure patients can continue and benefit from further treatment.6 Managing these AEs demands care from multiple specialists that form a multidisciplinary tumor board (MTB). Close collaboration and cooperation between specialties in the MTB fosters shared decision-making and can help to prevent serious AEs and drug toxicity. Conversely, lack of communication and coordination can lead to fragmented care with poor patient outcomes.6
Specialists managing treatment for patients with high-risk NMIBC may include:6
- Primary care doctors
- Pathologists
- Urologists
- Nurses
- Medical oncologists
- Rheumatologists
- Endocrinologists
- Respirologists
Preventing disease recurrence
In patients with high-risk NMIBC, delays in detecting tumors could lead to muscle invasion, and delays in introducing therapy can be life-threatening.4 One study (N=88) showed that rates of recurrence, progression, metastasis, and mortality rate were all significantly higher in patients with NMIBC who did not adhere to a standardized surveillance protocol compared with those who did.7 Hence, strict adherence to surveillance guidelines is strongly recommended, particularly for patients with high-risk NMIBC.7
These patients should undergo cystoscopy and cytology 3 to 4 months after transurethral resection of the bladder tumor (TURBT), repeated every 3–4 months for 2 years; every 6 months thereafter until 5 years; then annually.4,8
A positive or suspicious cystoscopy should trigger investigation for recurrence. TURBT and biopsies are recommended for abnormal-looking mucosa, as well as bladder random biopsies and a prostatic urethra biopsy if indicated.4 Upper tract imaging, enhanced cystoscopic techniques, and utereoscopy should also be considered.8
For more insights on recurrence and psychological support for NMIBC management, listen to our podcast with expert Alison Birtle and patient Melanie Costin.
References
- Jaromin, 2024. Revolutionizing treatment: Breakthrough approaches for BCG-unresponsive non-muscle-invasive bladder cancer. https://www.doi.org/10.3390/cancers16071366
- Li, 2024. Bladder-sparing therapy for Bacillus Calmette-Guérin–unresponsive non–muscle-invasive bladder cancer: International Bladder Cancer Group recommendations for optimal sequencing and patient selection. https://www.doi.org/10.1016/j.eururo.2024.08.001
- Grabe-Heyne, 2023. Intermediate and high-risk non-muscle-invasive bladder cancer: An overview of epidemiology, burden, and unmet needs. https://www.doi.org/10.3389/fonc.2023.1170124
- Gontero, 2024. European Association of Urology guidelines on mon-muscle-invasive bladder cancer (TaT1 and carcinoma in situ)—A summary of the 2024 guidelines update. https://www.doi.org/10.1016/j.eururo.2024.07.027
- Schubach, 2024. Identifying the supportive care needs of people affected by non-muscle invasive bladder cancer: An integrative systematic review. https://www.doi.org/10.1007/s11764-024-01558-7
- Black, 2024. The evolving role of PD-(L)1 inhibition in optimizing outcomes for high-risk non-muscle-invasive bladder cancer (NMIBC): A podcast. https://www.doi.org/10.1007/s12325-023-02763-z
- Abushamma, 2021. The impact of non-compliance to a standardized risk-adjusted protocol on recurrence, progression, and mortality in non-muscle invasive bladder cancer. https://www.doi.org/10.2147/cmar.s299148
- Chang, 2016. Diagnosis and treatment of non-muscle invasive bladder cancer: AUA/SUO guideline. https://www.doi.org/10.1016/j.juro.2016.06.049
Weighing up: Cystectomy versus bladder sparing
That was kind of a standout, as something that I think that we can impact.
What can healthcare professionals (HCPs) say to guide patients with non-muscle-invasive bladder cancer (NMIBC) facing a decision between complete bladder removal or a more conservative approach?
The CISTO trial investigated life after cystectomy versus bladder-sparing treatment to provide answers for HCPs and patients alike, but the results ran contrary to the researchers’ expectations.
Here, Stephanie Chisolm (Bladder Cancer Advocacy Network, Bethesda, Maryland, USA) and Janet Kukreja (University of Colorado Anschutz Medical Center, Aurora, USA) pick out the key findings and explain how they can provide information and reassurance to patients weighing up the pros and cons of the two treatment approaches.
Developed by EPG Health. This content has been developed independently of the sponsor, Pfizer, which has had no editorial input into the content. EPG Health received funding from the sponsor to help provide healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.

