Disease Management
There will be details of blood coagulation factors II, VII, IX and more; the coagulation cascade; haemorrhagic risk assessment, using the international normalised ratio; the factor Xa inhibitors rivaroxaban, edoxaban or apixaban; the factor IIa (thrombin) inhibitor dabigatran; the risks of warfarin treatment; current national and international guidelines; the use of fresh frozen plasma to reverse vitamin K antagonist (VKA) anticoagulation; plasma and rVIIA; and details of the anticoagulation reversal agents idarucizumab, andexanet alpha and ciraparantag are all included in this section.
Blood Coagulation
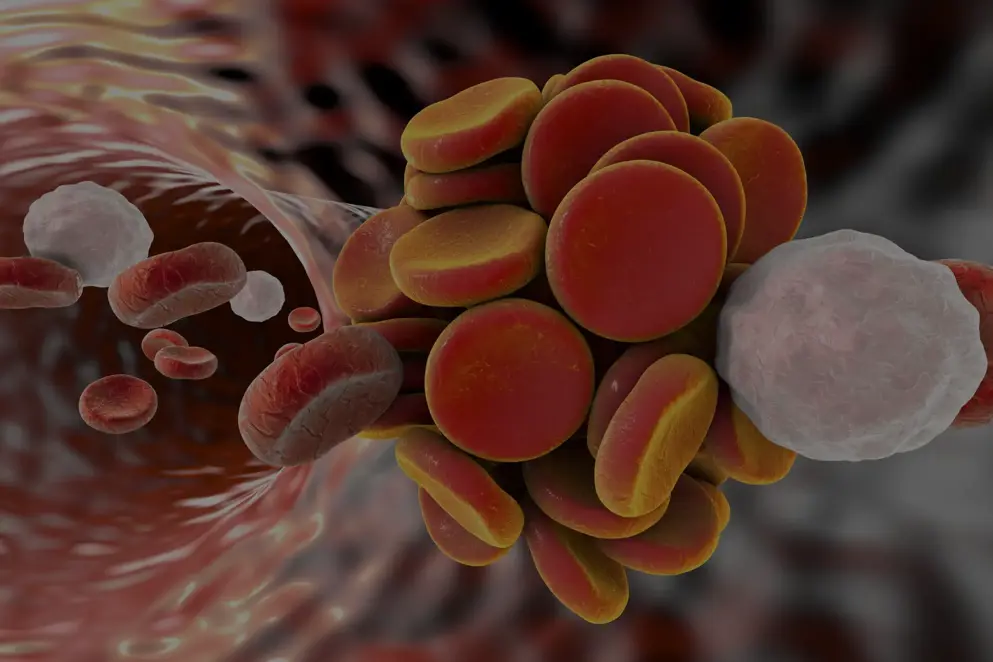
Blood coagulation involves the complex interaction of multiple factors resulting in the generation of an insoluble fibrin clot. Classically blood coagulation was considered to be a cascade involving two convergent pathways: the intrinsic (contact activation) pathway and the extrinsic (tissue factor) pathway. [Monroe and Hoffman 2006; Adams and Bird 2009; Alquwaizani et al., 2013] More recently, blood coagulation is considered to consist of phases, involving initiation, amplification, propagation and finally, clot stabilisation. [Monroe and Hoffman 2006; Adams and Bird 2009] {Figure 1}
A feature of blood coagulation is the activation of multiple inert proenzymes and cofactors (indicated by “a” after the clotting factor numeral), with binding to cell surfaces localising these factors and enzymatic reactions. In the initiation phase, a complex of the transmembrane glycoprotein tissue factor and activated factor VII (FVIIa) activates factors IX and X. Factor Xa, which is bound to tissue factor expressing cells such as fibroblasts and platelets, then generates a small amount of thrombin (FIIa) from prothrombin (FII). The amplification phase involves thrombin activation of platelets, and also of platelet-bound factors V, VIII and XI. This generates increasing amounts of thrombin required for the propagation phase in which fibrin is generated by the catalysis of fibrinogen. A stable fibrin clot is formed following cross linkage of fibrin polymers with factor XIIIa. [Monroe and Hoffman 2006; Adams and Bird 2009]
Figure 1. Outline of the phases of blood coagulation. (CSL Behring, based on Monroe and Hoffman, 2006).
TF, tissue factor; vWF, von Willebrand factor.
of interest
are looking at
saved
next event
Disease Management References
Abraham NS, Singh S, Alexander GC, Heien H, Haas LR, Crown W, et al. Comparative risk of gastrointestinal bleeding with dabigatran, rivaroxaban, and warfarin. BMJ. 2015;350:h1857.
Adams RL, Bird RJ. Coagulation cascade and therapeutics update: relevance to nephrology. Part 1: Overview of coagulation, thrombophilias and history of anticoagulants. Nephrology (Carlton). 2009;14:462-70.
Ageno W, Büller HR, Falanga A, Hacke W, Hendriks J, Lobban T, et al. Managing reversal of direct oral anticoagulants in emergency situations. Anticoagulation Education Task Force White Paper. Thromb Haemost. 2016;116(6):1003-10.
Alquwaizani M, Buckley L, Adams C, Fanikos J. Anticoagulants: A Review of the Pharmacology, Dosing, and Complications. Curr Emerg Hosp Med Rep. 2013;1:83-97.
Ansell JE, Bakhru SH, Laulicht BE, Steiner SS, Grosso M, Brown K, et al. Use of PER977 to reverse the anticoagulant effect of edoxaban. N Engl J Med. 2014;371:2141-2.
Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G, et al. Pharmacology and management of the vitamin K antagonists: American College of Chest. Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133:160S-198S.
Ansell J, Hirsh J, Poller L, Bussey H, Jacobson A, Hylek E. The pharmacology and management of the vitamin K antagonists: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:204S-33S.
Appleby N, Groarke E, Crowley M, Wahab FA, McCann AM, Egan L, et al. Reversal of warfarin anticoagulation using prothrombin complex concentrate at 25 IU kg-1 : results of the RAPID study. Transfus Med. 2016 Oct 7. doi: 10.1111/tme.12371. [Epub ahead of print]
Baglin T, Hillarp A, Tripodi A, Elalamy I, Buller H, Ageno W. Measuring Oral Direct Inhibitors (ODIs) of thrombin and factor Xa: A recommendation from the Subcommittee on Control of Anticoagulation of the Scientific and Standardisation Committee of the International Society on Thrombosis and Haemostasis. J Thromb Haemost. 2013;11:756-60.
Baharoglu MI, Cordonnier C, Salman RA, de Gans K, Koopman MM, Brand A, et al. Platelet transfusion versus standard care after acute stroke due to spontaneous cerebral haemorrhage associated with antiplatelet therapy (PATCH): a randomised, open-label, phase 3 trial. Lancet. 2016 May 9. pii: S0140-6736(16)30392-0. [Epub ahead of print]
Barco S, Cheung YW, Coppens M, Hutten BA, Meijers JC, Middeldorp S. In vivo reversal of the anticoagulant effect of rivaroxaban with four-factor prothrombin complex concentrate. Br J Haematol. 2016;172:255-61.
Batchelor JS, Grayson A. A meta-analysis to determine the effect on survival of platelet transfusions in patients with either spontaneous or traumatic antiplatelet medication-associated intracranial haemorrhage. BMJ Open. 2012;2:e000588.
Beyer-Westendorf J, Förster K, Pannach S, Ebertz F, Gelbricht V, Thieme C, et al. Rates, management, and outcome of rivaroxaban bleeding in daily care: results from the Dresden NOAC registry. Blood. 2014;124:955-62.
Boulis NM, Bobek MP, Schmaier A, Hoff JT. Use of factor IX complex in warfarin-related intracranial hemorrhage. Neurosurgery 1999;45:1113-8.
Burr N, Lummis K, Sood R, Kane JS, Corp A, Subramaniam V. Risk of gastrointestinal bleeding with direct oral anticoagulants: a systematic review and network meta-analysis. Lancet Gasteroenterol Hepatol. 2017;2:85-93.
Caldeira D, Barra M, Ferreira A, Rocha A, Augusto A, Pinto FJ, et al. Systematic review with meta-analysis: the risk of major gastrointestinal bleeding with non-vitamin K antagonist oral anticoagulants. Aliment Pharmacol Ther. 2015;42:1239-49.
Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Europace. 2010;12:1360-420.
Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH et al. Focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33:2719-47
Camm AJ, Pinto FJ, Hankey GJ, Andreotti F, Hobbs FD; Writing Committee of the Action for Stroke Prevention alliance. Non-vitamin K antagonist oral anticoagulants and atrial fibrillation guidelines in practice: barriers to and strategies for optimal implementation. Europace. 2015;17:1007-17.
Cannegieter SC, Rosendaal FR, Wintzen AR, van der Meer FJ, Vandenbroucke JP, Briët E. Optimal oral anticoagulant therapy in patients with mechanical heart valves. N Engl J Med. 1995;333:11-7.
Carothers C, Giancarelli A, Ibrahim J, Hobbs B. Activated prothrombin complex concentrate for warfarin reversal in traumatic intracranial hemorrhage. J Surg Res. 2018;223:183-7.
Chai-Adisaksopha C, Hillis C, Siegal DM, Movilla R, Heddle N, Iorio A, et al. Prothrombin complex concentrates versus fresh frozen plasma for warfarin reversal. A systematic review and meta-analysis. Thromb Haemost. 2016;116(5):879-90.
Chang HY, Zhou M, Tang W, Alexander GC, Singh S. Risk of gastrointestinal bleeding associated with oral anticoagulants: population based retrospective cohort study. BMJ. 2015;350:h1585.
Cheung YW, Barco S, Hutten BA, Meijers JC, Middeldorp S, Coppens M. In vivo increase in thrombin generation by four-factor prothrombin complex concentrate in apixaban-treated healthy volunteers. J Thromb Haemost. 2015;13:1799-805.
Cheung KS, Leung WK. Gastrointestinal bleeding in patients on novel oral anticoagulants: risk, prevention and management. World J Gasteroenterol. 2017;23:1954-63.
Crowther MA, Warkentin TE. Bleeding risk and the management of bleeding complications in patients undergoing anticoagulant therapy: focus on new anticoagulant agents. Blood. 2008;111:4871-9.
CSL Behring. Factors for Life. Available from: http://www.cslbehring.com/docs/578/927/CSL%20Behring%20Factors%20for%20Life_Coagulation%20Disorders.pdf. (Accessed 8 January 2016).
Das A, Liu D. Novel antidotes for target specific oral anticoagulants. Exp Hematol Oncol. 2015;15;4:25.
DeAngelo J, Jarell D, Cosgrove R, Camamo J, Edwards C, Patanwala AE. Comparison of 3-factor versus 4-factor prothrombin complex concentrate with regard to warfarin reversal, blood product use, and costs. Am J Ther. 2017; [epub ahead of print].
Demeyere R, Gillardin S, Arnout J, Strengers PF. Comparison of fresh frozen plasma and prothrombin complex concentrate for the reversal of oral anticoagulants in patients undergoing cardiopulmonary bypass surgery: a randomized study. Vox Sang. 2010;99:251-60.
de Oliveira Manoel AL, Goffi A, Zampieri FG, Turkel-Parrella D, Duggal A, Marotta TR, Macdonald RL, et al. The critical care management of spontaneous intracranial hemorrhage: a contemporary review. Crit Care. 2016;20:272.
Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, et al. Perioperative management of antithrombotic therapy. Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest. Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e326S-350S.
Eerenberg ES, Kamphuisen PW, Sijpkens MK, Meijers JC, Buller HR, Levi M. Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: a randomized, placebo-controlled, crossover study in healthy subjects. Circulation. 2011;124:1573-9.
European Medicines Agency. EMA fast-tracks antidote to anticoagulant Pradaxa. September 2015a; Available from: http://www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2015/09/news_detail_002399.jsp&mid=WC0b01ac058004d5c1 (Accessed 5 February 2016).
European Medicines Agency. Summary of Product Characteristics. Praxbind. December 2015b; Available from: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/003986/human_med_001938.jsp&mid=WC0b01ac058001d124 (Accessed 5 February 2016).
Evans G, Luddington R, Baglin T. Beriplex P/N reverses severe warfarin-induced over anticoagulation immediately and completely in patients presenting with major bleeding. Br J Haematol. 2001;115:998-1001.
Faraoni D, Levy JH, Albaladejo P, Samama CM; Groupe d’Intérêt en Hémostase Périopératoire. Updates in the perioperative and emergency management of non-vitamin K antagonist oral anticoagulants. Crit Care. 2015;19:203.
FDA, 2015. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2015/761025Orig1s000Approv.pdf (accessed October 2018).
FDA, 2018. Available from: https://www.fda.gov/downloads/BiologicsBloodVaccines/CellularGeneTherapyProducts/ApprovedProducts/UCM606687.pdf (accessed October 2018).
Frontera JA, Lewin III JJ, Rabinstein AA, Aisiku IP, Alexandrov AW, Cook AM, et al. Guideline for Reversal of Antithrombotics in Intracranial Hemorrhage: A Statement for Healthcare Professionals from the Neurocritical Care Society and Society of Critical Care Medicine. Neurocrit Care. 2016;24(1):6-46.
German Medical Association. Cross-sectional guidelines for therapy with blood components and blood derivatives; plasma for therapeutic use. Transfus Med Hemother. 2009;36:345–492.
Ghanny S, Warkentin TE, Crowther MA. Reversing anticoagulant therapy. Curr Drug Discov Technol. 2012;9:143-9.
Ghate SR, Biskupiak J, Ye X, Kwong WJ, Brixner DI. All-cause and bleeding-related health care costs in warfarin-treated patients with atrial fibrillation. J Manag Care Pharm 2011;17:672-84.
Glund S, Stangier J, Schmohl M, Gansser D, Norris S, van Ryn J, et al. Safety, tolerability, and efficacy of idarucizumab for the reversal of the anticoagulant effect of dabigatran in healthy male volunteers: a randomised, placebo-controlled, double-blind phase 1 trial. Lancet. 2015;386:680-90.
Goldstein JN, Refaai MA, Milling TJ Jr, Lewis B, Goldberg-Alberts R, et al. Four-factor prothrombin complex concentrate versus plasma for rapid vitamin K antagonist reversal in patients needing urgent surgical or invasive interventions: a phase 3b, open-label, non-inferiority, randomised trial. Lancet. 2015;385(9982):2077-87.
Graham DJ, Reichman ME, Wernecke M, Zhang R, Southworth MR, Levenson M, et al. Cardiovascular, bleeding, and mortality risks in elderly Medicare patients treated with dabigatran or warfarin for nonvalvular atrial fibrillation. Circulation. 2015;131:157-64.
Grandhi R, Newman WC, Zhang X, Harrison G, Moran C, Okonkwo DO, et al. Administration of 4-Factor Prothrombin Complex Concentrate as an Antidote for Intracranial Bleeding in Patients Taking Direct Factor Xa Inhibitors. World Neurosurg. 2015;84:1956-61.
Green L, Tan J, Morris JK, Alikhan R, Curry N, Everington T, et al. A three-year prospective study of the presentation and clinical outcomes of major bleeding episodes associated with oral anticoagulant use in the UK (ORANGE study). Haematologica. 2018;103:738-45.
Grottke O, Van Ryn J, Spronk HM, Rossaint R. Prothrombin complex concentrates and a specific antidote to dabigatran are effective ex-vivo in reversing the effects of dabigatran in an anticoagulation/ liver trauma experimental model. Crit Care. 2014;18:R27.
Grottke O, Aisenberg J, Bernstein R, Goldstein P, Huisman MV, Jamieson DG, et al. Efficacy of prothrombin complex concentrates for the emergency reversal of dabigatran-induced anticoagulation. Crit Care. 2016;20(1):115.
Hanley JP. Warfarin reversal. J Clin Pathol. 2004;57:1132-9.
Harter K, Levine M, Henderson SO. Anticoagulation drug therapy: a review. West J Emerg Med. 2015;16:11-7.
Herzog E, Kaspereit FJ, Krege W, Doerr B, van Ryn J, Dickneite G, et al. Thrombotic safety of prothrombin complex concentrate (Beriplex P/N) for dabigatran reversal in a rabbit model. Thromb Res. 2014;134:729-36.
Herzog E, Kaspereit F, Krege W, Doerr B, Mueller-Cohrs J, Pragst I, et al. Effective reversal of edoxaban-associated bleeding with four-factor prothrombin complex concentrate in a rabbit model of acute hemorrhage. Anesthesiology. 2015a;122:387-98.
Herzog E, Kaspereit F, Krege W, Mueller-Cohrs J, Doerr B, Niebl P, et al. Correlation of coagulation markers and 4F-PCC-mediated reversal of rivaroxaban in a rabbit model of acute bleeding. Thromb Res. 2015b;135:554-60.
Herzog E, Kaspereit F, Krege W, Mueller-Cohrs J, Doerr B, Niebl P, et al. Four-factor prothrombin complex concentrate reverses apixaban-associated bleeding in a rabbit model of acute hemorrhage. J Thromb Haemost. 2015c;13:2220-6.
Hirsh J, Fuster V, Ansell J, Halperin JL; American Heart Association/American College of Cardiology Foundation. American Heart Association/ American College of Cardiology Foundation guide to warfarin therapy. J Am Coll Cardiol. 2003;41:1633-52.
Holbrook A, Schulman S, Witt DM, Vandvik PO, Fish J, Kovacs MJ, et al. Evidence-based management of anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest. Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e152S-84S.
Holt T, Taylor S, Abraham P, McMillan W, Harris S, Curtis J, Elder T et al. Three- versus four-factor prothrombin complex concentrate for the reversal of warfarin-induced bleeding. Int J Crit Illn Inj Sci. 2018;8:36-40.
Honickel M, Braunschweig T, van Ryn J, Ten Cate H, Spronk HM, Rossaint R, et al. Prothrombin complex concentrate is effective in treating the anticoagulant effects of dabigatran in a porcine polytrauma model. Anesthesiology. 2015;123(6):1350-61.
Imberti D, Barillari G, Biasioli C, Bianchi M, Contino L, Duce R, et al. Emergency reversal of anticoagulation with a three-factor prothrombin complex concentrate in patients with intracranial haemorrhage. Blood Transfus. 2011;9:148-55.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64:e1-76.
Johansen M, Wikkelsø A, Lunde J, Wetterslev J, Afshari A. Prothrombin complex concentrate for reversal of vitamin K antagonist treatment in bleeding and non-bleeding patients. Cochrane Database Syst Rev. 2015;7:CD010555.
Kaatz S, Kouides PA, Garcia DA, Spyropolous AC, Crowther M, Douketis JD, et al. Guidance on the emergent reversal of oral thrombin and factor Xa inhibitors. Am J Hematol. 2012;87(Suppl 1):S141-5.
Keeling D, Baglin T, Tait C, Perry D, Baglin C, Kitchen S, et al. Guidelines on oral anticoagulation with warfarin - fourth edition. Br J Haematol. 2011;154:311-24.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37:2893-962.
Kozek-Langenecker SA, Ahmed A, Afshari A, Albaladejo P, Aldecoa P, Barauskas G, et al. Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol. 2017;34:332-95.
Landefeld CS, Beyth RJ. Anticoagulant-related bleeding: clinical epidemiology, prediction, and prevention. Am J Med. 1993;95:315-28.
Lankiewicz MW, Hays J, Friedman KD, Tinkoff G, Blatt PM. Urgent reversal of warfarin with prothrombin complex concentrate. J Thromb Haemost. 2006;4:967-70.
Lazo-Langner A, Lang ES, Douketis J. Clinical review: Clinical management of new oral anticoagulants: a structured review with emphasis on the reversal of bleeding complications. Crit Care. 2013;17:230.
Levi M, Moore KT, Castillejos CF, Kubitza D, Berkowitz SD, Goldhaber SZ, et al. Comparison of three-factor and four-factor prothrombin complex concentrates regarding reversal of the anticoagulant effects of rivaroxaban in healthy volunteers. J Thromb Haemost. 2014;12(9):1428-36.
Levine MN, Raskob G, Beyth RJ, Kearon C, Schulman S. Hemorrhagic complications of anticoagulant treatment: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:287S-310S.
Levy JH, Tanaka KA, Dietrich W. Perioperative hemostatic management of patients treated with vitamin K antagonists. Anesthesiology. 2008;109:918-26.
Lip GY, Windecker S, Huber K, Kirchhof P, Marin F, Ten Berg JM, et al. Management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous coronary or valve interventions: a join consensus document of the European Society of Cardiology Working Group on Thrombosis, European Heart Rhythm Association (EHRA), European Association of Percutaneous Cardiovascular Interventions (EAPCI) and European Association of Acute Cardiac Care (ACCA) endorsed by the Heart Rhythm Society (HRS) and Asia-Pacific Heart Rhythm Society (APHRS). Eur Heart J. 2014;35:3155-79.
Majeed A, Meijer K, Larrazabal R, Arnberg F, Luijckx GJ, Roberts RS, et al. Mortality in vitamin K antagonist-related intracerebral bleeding treated with plasma or 4-factor prothrombin complex concentrate. Thromb Haemost. 2014;111:233-9.
Makris M, Watson HG. Annotation: The management of coumarin-induced over-anticoagulation. Br J Haematol. 2001;114:271-80.
Milling TJ Jr, Kaatz S. Preclinical and Clinical Data for Factor Xa and "Universal" Reversal Agents. Am J Med. 2016;129(11S):S80-S8.
Milling TJ Jr, Refaai MA, Goldstein JN, Schneider A, Omert L, Harman A, et al. Thromboembolic Events After Vitamin K Antagonist Reversal With 4-Factor Prothrombin Complex Concentrate: Exploratory Analyses of Two Randomized, Plasma-Controlled Studies. Ann Emerg Med. 2016;67:96-105.e5.
Monroe DM, Hoffman M. What does it take to make the perfect clot? Arterioscler Thromb Vasc Biol. 2006;26:41-8.
Pabinger I, Brenner B, Kalina U, Knaub S, Nagy A, Ostermann H, et al. Prothrombin complex concentrate (Beriplex® P/N) for emergency anticoagulation reversal: a prospective multinational clinical trial. J Thromb Haemost. 2008;6:622-31.
Pabinger I, Tiede A, Kalina U, Knaub S, Germann R, Ostermann H, et al. Impact of infusion speed on the safety and effectiveness of prothrombin complex concentrate: a prospective clinical trial of emergency anticoagulation reversal. Ann Hematol. 2010;89:309-16.
Palareti G, Leali N, Coccheri S, Poggi M, Manotti C, D'Angelo A, et al. Bleeding complications of oral anticoagulant treatment:an inception-cohort, prospective collaborative study (ISCOAT). Italian Study on Complications of Oral Anticoagulant Therapy. Lancet. 1996;348:423-8.
Pengo V, Crippa L, Falanga A, Finazzi G, Marongiu F, Palareti G, et al. Questions and answers on the use of dabigatran and perspectives on the use of other new oral anticoagulants in patients with atrial fibrillation. A consensus document of the Italian Federation of Thrombosis Centers (FCSA). Thromb Haemost. 2011;106:868-76.
Pernod G, Godier A, Gozalo C, Tremey B, Sié P; French National Authority for Health. French clinical practice guidelines on the management of patients on vitamin K antagonists in at-risk situations (overdose, risk of bleeding, and active bleeding). Thromb Res. 2010;126:e167-74.
Pernod G, Albaladejo P, Godier A, Samama CM, Susen S, Gruel Y, et al. Management of major bleeding complications and emergency surgery in patients on long-term treatment with direct oral anticoagulants, thrombin or factor-Xa inhibitors: proposals of the working group on perioperative haemostasis (GIHP) - March 2013. Arch Cardiovasc Dis. 2013;106:382-93.
Pollack CV Jr, Reilly PA, Eikelboom J, Glund S, Verhamme P, Bernstein RA, et al. Idarucizumab for dabigatran reversal. N Engl J Med. 2015;373:511-20.
Pollack CV, Reilly PA, van Ryn J, Eikelboom JW, Glund S, Bernstein RA, et al. Idarucizumab for dabigatran reversal – full cohort analysis. New Engl J Med. 2017;377:431-41.
Portola Pharmaceuticals. Press release. Portola Pharmaceuticals Announces New Interim Results from Ongoing ANNEXA-4 Study of Factor Xa Inhibitor Reversal Agent AndexXa® (Andexanet Alfa) in Patients with Life-Threatening Bleeding. Available at: https://globenewswire.com/news-release/2018/03/12/1420761/0/en/Portola-Pharmaceuticals-Announces-New-Interim-Results-from-Ongoing-ANNEXA-4-Study-of-Factor-Xa-Inhibitor-Reversal-Agent-AndexXa-Andexanet-Alfa-in-Patients-with-Life-Threatening-Ble.html (accessed April 2018).
Purrucker JC, Haas K, Rizos T, Khan S, Wolf M, Hennerici MG, et al. Early Clinical and Radiological Course, Management, and Outcome of Intracerebral Hemorrhage Related to New Oral Anticoagulants. JAMA Neurol. 2016;73(2):169-77.
Radaelli F, Dentali F, Repici A, Amato A, Paggi S, Rondonotti E, et al. Management of anticoagulation in patients with acute gastrointestinal bleeding. Dig Liver Dis. 2015;47:621-7.
Refaai MA, Goldstein JN, Lee ML, Durn BL, Milling TJ Jr, Sarode R. Increased risk of volume overload with plasma compared with four-factor prothrombin complex concentrate for urgent vitamin K antagonist reversal. Transfusion. 2015;55:2722-9.
Roussaint R, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, et al. The European guideline on the management of major bleeding and coagulopathy following trauma: fourth edition. Crit Care. 2016;20:100.
Sarode R, Milling TJ Jr, Refaai MA, Mangione A, Schneider A, Durn BL, et al. Efficacy and safety of a 4-factor prothrombin complex concentrate in patients on vitamin K antagonists presenting with major bleeding: a randomized, plasma-controlled, phase IIIb study. Circulation. 2013;128:1234-43.
Schick KS, Fertmann JM, Jauch KW, Hoffmann JN. Prothrombin complex concentrate in surgical patients: retrospective evaluation of vitamin K antagonist reversal and treatment of severe bleeding. Crit Care. 2009;13:R191.
Siegal DM. Managing target-specific oral anticoagulant associated bleeding including an update on pharmacological reversal agents. J Thromb Thrombolysis. 2015;39:395-402.
Siegal DM, Curnutte JT, Connolly SJ, Lu G, Conley PB, Wiens BL, et al. Andexanet Alfa for the Reversal of Factor Xa Inhibitor Activity. N Engl J Med. 2015;373:2413-24.
Steffel J, Verhamme P, Potpara TS, Albaladejo P, Antz M, Desteghe L, et al. The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J. 2018; [epub ahead of print].
Steinhubl SR, Bhatt DL, Brennan DM, Montalescot G, Hankey GJ, Eikelboom JW, et al. Aspirin to prevent cardiovascular disease: the association of aspirin dose and clopidogrel with thrombosis and bleeding. Ann Intern Med. 2009;150:379-86.
Suzuki Y, Kitahara T, Soma K, Konno S, Sato K, Suzuki S, et al. Impact of platelet transfusion on survival of patients with intracerebral hemorrhage after administration of anti-platelet agents at a tertiary emergency center. PLoS One. 2014;9:e97328.
US Food and Drug Administration, 2018. Available from: https://www.fda.gov/downloads/BiologicsBloodVaccines/CellularGeneTherapyProducts/ApprovedProducts/UCM606687.pdf (accessed October 2018).
US National Library of Medicine. Available from: https://clinicaltrials.gov/ct2/show/NCT01826266 (accessed April 2018).
van der Meer FJ, Rosendaal FR, Vandenbroucke JP, Briët E. Bleeding complications in oral anticoagulant therapy. An analysis of risk factors. Arch Intern Med. 1993;153:1557-62.
van Ryn J, Schurer J, Kink-Eiband M, Clemens A. Reversal of dabigatran-induced bleeding by coagulation factor concentrates in a rat-tail bleeding model and lack of effect on assays of coagulation. Anesthesiology. 2014;120:1429-40.
Xu W, Hu S, Wu T. Risk analysis of new oral anticoagulants for gastrointestinal bleeding and intracranial hemorrhage in atrial fibrillation patients: a systematic review and network meta-analysis. J Zhejiang Univ-Sci B (Biomed & Biotechnol). 2017;18:567-76.
Zahir H, Brown KS, Vandell AG, Desai M, Maa JF, Dishy V, et al. Edoxaban effects on bleeding following punch biopsy and reversal by a 4-factor prothrombin complex concentrate. Circulation. 2015;131:82-90.
of interest
are looking at
saved
next event
Job number: KCT16-01-0010
Developed by EPG Health for Medthority in collaboration with CSL Behring, with content provided by CSL Behring.
Not intended for Healthcare Professionals outside Europe.

