Guidelines
Keep up to date with the latest guidelines and compare your own clinical practice against expert recommendations in this section of the Oral Anticoagulation Reversal Learning Zone.
The American College of Surgeons’ Guidelines for the Perioperative Management of Antithrombotic Medication
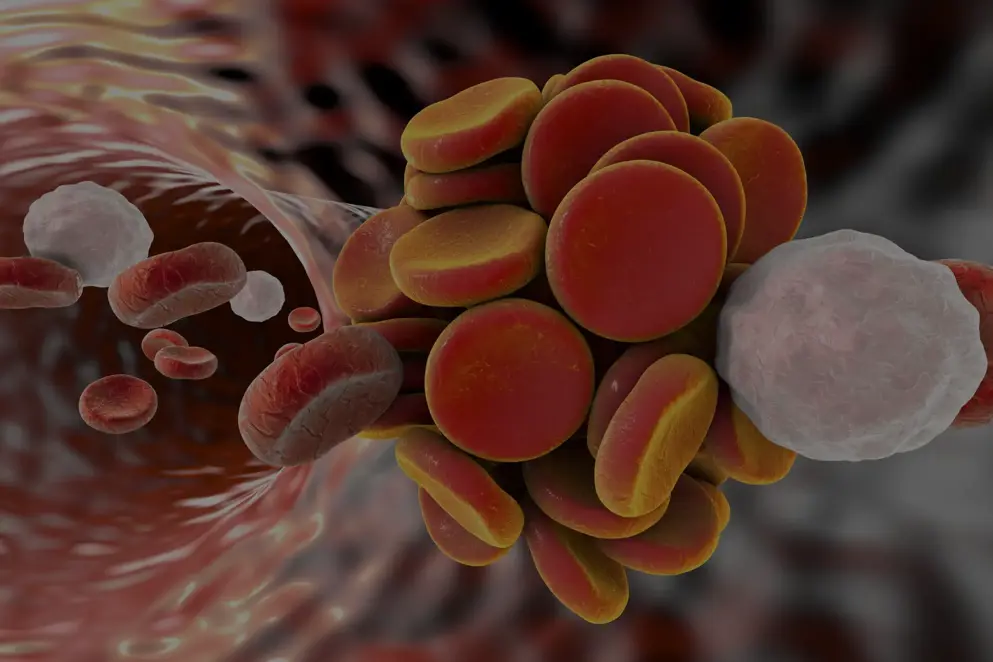
Antithrombotic therapy has become increasingly necessary due to the ageing global population and the rise of chronic medical conditions that come with an increased risk of thrombosis. Patients typically prescribed antithrombotic therapies are also more likely to require surgery with 1 in 10 surgical patients prescribed chronic anticoagulation therapy (Roger et al., 2012). Dual agent antiplatelet therapy is also being commonly prescribed for the secondary prevention of myocardial infarction and stent thrombosis (Hornor et al., 2018).
Managing these chronic conditions perioperatively can prove challenging, as a balance needs to be found between operative bleeding risk and thromboembolic risk when deciding to stop and restart antithrombotic medications.
Recently published guidelines from the American College of Surgeons (ACS) provide recommendations on the perioperative management of antithrombotic medication. These guidelines are intended to update, summarise, and combine existing guidelines, and cover five topics: thromboembolic risk from discontinuing antithrombotic agents, determining the bleeding risk of surgical procedures and patient characteristics, the timing and appropriateness of heparin bridging, management strategies for elective surgery, and considerations for the nonelective surgical setting (Hornor et al., 2018). Learn more about each section of the guidelines in our interactive summary below.
Estimating thromboembolic risk
Discontinuing antithrombotic therapy to avoid the risk of major bleeding during surgery is common practice around the world. However, understanding the risks of stopping antithrombotic medication is paramount to surgical practice, as the risk of clinical harm due to thrombotic events is believed to be higher than those of major perioperative bleeding (figure 1).
Figure 1. Fatality and mortality rates due to thrombotic and major bleeding events (Deviri et al., 1991; Feigin et al., 2014; Wu et al., 2014; Wu et al., 2015).
VTE, venous thromboembolism
This is why the American College of Surgeons’ (ACS) guidelines recommend assessing thromboembolic risk as the first step in developing a perioperative antithrombotic management strategy (Hornor et al., 2018).
The ACS guidelines have stratified thromboembolic risk into high (>10%), moderate (5–10%), and low (<5%) categories and are adapted from the 9th Edition of the American College of Chest Physicians’ (CHEST) guidelines (Douketis et al., 2012).
Thromboembolic risk should be considered on an individual basis and is dependent on several patient factors, the most important of which is the medical indication of the antithrombotic agent. These guidelines discuss the risks of several conditions that require the use of chronic anticoagulation, including nonvalvular atrial fibrillation, prosthetic heart valves, venous thromboembolism, coronary artery disease, stroke, and peripheral arterial disease.
Nonvalvular atrial fibrillation
The CHA2DS2-VASc score is a tool often used to predict the likelihood of a stroke occurring in patients with non-rheumatic atrial fibrillation. It is recommended that the calculated score be used to categorise patients into low, moderate or high thromboembolic risk (figure 2) (Friberg et al., 2012).
Figure 2. The CHA2DS2-VASc score can be stratified into three categories of thromboembolic risk (Hornor et al., 2018).
It is important to note that the CHA2DS2-VASc score hasn’t been prospectively validated in the perioperative setting, however, it has been used to estimate thromboembolic risk if anticoagulation is held and to determine whether heparin bridging is indicated perioperatively.
Prosthetic heart valves
When assessing the perioperative thromboembolic risk in patients with prosthetic heart valves, there are a number of elements to take into consideration, such as the
- type
- number
- location of the valvular prosthetic
- as well as the presence of additional cardiac risk factors
-
such as atrial fibrillation, previous stroke or transient ischemic attack, hypertension, diabetes, congestive heart failure, age >75 years (Whitlock et al., 2012)
-
Figure 3. Thromboembolic risk when anticoagulated with warfarin according to prosthetic heart valve type (Cannegieter et al., 1994; Whitlock et al., 2012; Hornor et al., 2018).
Bioprosthetic valves
Bioprosthetic heart valves do not require long-term anticoagulation for the valve alone; many guidelines recommend short-term anticoagulation after implantation (3–6 months) to decrease the incidence of thromboembolic events. If a patient is receiving anticoagulation after this period, then it is likely for a secondary reason and this should be factored into a risk/benefit analysis for stopping anticoagulation (Vahanian et al., 2012; Whitlock et al., 2012).
Elective operations should be delayed 3–6 months after implantation of a bioprosthetic valve.
In the case of nonelective operations, the surgeon should have no hesitancy stopping warfarin without any bridging methodology and restarting anticoagulation when there is no increased risk of bleeding (Whitlock et al., 2012).
Venous thromboembolism
Premature cessation of anticoagulation in the first three months after an acute venous thromboembolism (VTE) event has been shown to be associated with a 1-month risk of recurrent VTE of 40%, and a 10% risk for the subsequent 2 months. Annual risk of VTE falls to 15% after 3 months of anticoagulation (Research Committee of the British Thoracic Society, 1992; Levine et al., 1995). It is therefore recommended that elective surgery is postponed for 3 months following a diagnosis of VTE (Douketis et al., 2012).
The risk of VTE reoccurrence is also dependent of whether the VTE was provoked or unprovoked, and if there are any underlying risk factors such as cancer or inherited thrombophilia (de Jong et al., 2012). A provoked VTE is classified as an identifiable factor such as an inciting event (surgery, a long flight, hospital admission), transient major risk factors (major surgery, >30 minutes hospitalisation or immobility, pregnancy, oestrogen therapy), or permanent risk factors (inherited thrombophilia, chronic heart failure, inflammatory bowel disease, malignancy) (Kearon et al., 2016).
Figure 4. Thromboembolic risk in patients with a history of VTE (Bates et al., 2012; Hornor et al., 2018).
VTE, Venous thromboembolism
The ACS guidelines recommends close consultation with the prescribing physician when developing a perioperative anticoagulation strategy for patients with a history of an unprovoked VTE or a provoked/unprovoked life-threatening pulmonary embolism (de Jong et al., 2012; Hornor et al., 2018).
Coronary artery disease
For some patients with coronary artery disease, stent implantation via surgery is the most effective option. However, following stent implantation patients are at risk of stent thrombosis, with the risk being highest in the following 4–6. One strong risk factor for stent thrombosis is the discontinuation of dual antiplatelet therapy (Iakovou et al., 2005).
It is currently recommended that dual agent antiplatelet therapy is prescribed for at least 6–12 months after placement of bare-metal stents and drug-eluting stents (Kleiman, 2012). Therefore, when considering the discontinuation of antiplatelet therapy prematurely in patients with coronary artery disease, the risk of cardiac complications needs to be carefully weighed against major surgical bleeding risk. This is a consideration often needed as 5% of patients with coronary stents require non-cardiac surgery within 1 year of coronary stent implantations, rising to 23% within 5 years (Savonitto et al., 2011).
Figure 5. Recommended delays in elective surgery following stent placement (Fleisher et al., 2014; Hornor et al., 2018).
If surgery can’t be deferred a discussion should be had with the prescribing cardiologist regarding the risk/benefit ratio of stopping antiplatelet therapy and patient disclosure should be documented (Fleisher et al., 2014).
Stroke
Recent history of stroke has been significantly associated with major cardiovascular events after elective non-cardiac surgery (stroke within 3 months, OR 14.23; 95% CI 11.61–17.45). However, the risk plateaued at 9 months after a stroke (Jørgensen et al., 2014) and, therefore, elective surgery is recommended to be deferred at least 9 months after ischaemic stroke (Hornor et al., 2018).
Peripheral arterial disease
Pharmacological treatment of peripheral arterial disease (PAD) with dual antiplatelet therapy is recommended for patients who have ischaemic limb symptoms and clinically significant coronary or cerebrovascular disease. For patients with PAD without clinically significant coronary or cardiovascular disease a single agent such as aspirin, clopidogrel, or ticagrelor is recommended (Gerhard-Herman et al., 2017).
Figure 6. Patients with PAD considered high risk for perioperative thromboembolism (Hornor et al., 2018).
Antithrombotic medication should be managed accordingly in those considered high risk, and patients who receive antithrombotic medications for symptomatic PAD should be managed in close consultation with a vascular specialist or vascular surgeon.
The underlying health issues associated with antithrombotic complications play a major factor in assessing risk, but procedural risk also has a large influence on the chosen management strategies. Learn more about procedural risks in the next section of the ACS guidelines.
Procedural bleeding risk
After considering the thromboembolic risks of discontinuing anticoagulation in preparation for surgery, the American College of Surgeons’ (ACS) guidelines next recommend considering the risks associated with the surgical procedure (Hornor et al., 2018). The invasiveness of the surgery, consequences of bleeding, and the patient’s medical history including any comorbidities that may affect coagulation are all important factors to consider (Tafur et al., 2012).
Patient characteristics
Recording a detailed medical history will reveal patient characteristics that increase bleeding risk. When asking for a patient’s medical history there should be a focus on previous surgery, trauma, family history, and current antithrombotic medications (Chee et al., 2008).
One way to assess bleeding risk based on patient characteristics is by calculating the HAS-BLED score (Hypertension, Abnormal renal/liver function, Stroke, Bleeding history or predisposition, Labile INR, Elderly, Drugs/alcohol concomitantly) (figure 1). This tool has been shown to be a valid and reliable predictor of bleeding events during perioperative heparin bridging of chronic oral anticoagulation (Omran et al., 2012; Roldán et al., 2013).
Figure 1. The HAS-BLED tool (Hornor et al., 2018).
ALT, Alanine aminotransferase; AP, Alkaline phosphate; AST, Aspartate aminotransferase; Cr, Creatinine; INR, International normalised ratio; NSAIDs, Nonsteroidal anti-inflammatory drugs
Procedural bleeding risk
Certain minimally invasive procedures do not require the discontinuation of antithrombotic agents:
- dental extraction
- cataract removal
- joint injections
- diagnostic endoscopic procedures
However, some guidelines and reviews have grouped procedures into lower or higher bleeding risk categories (Veitch et al., 2008; Baron et al., 2013; Spyropoulos et al., 2016).
Due to limited evidence surrounding periprocedural bleeding risk, the ACS guidelines recommend that bleeding risk due to the procedure or operation should be assessed on an individual basis by the surgeon, making a judgement based on their own experience. Postoperative physical examination of wounds and haematomas should inform the safety of resuming antithrombotic therapy (Hornor et al., 2018).
After considering the risks associated with procedural bleeding and the thromboembolic risks of stopping antithrombotic medications, the next step the ACS guidelines discuss is when heparin bridging should be considered. Find out if your practice is in line with these recommendations in the next section of the guidelines.
Perioperative heparin bridging
Before carrying out surgical procedures, it is often necessary to bridge anticoagulation therapy to minimise the risk of venous thromboembolism (VTE) and the risk of bleeding associated with high-risk procedures. The bridging process works by substituting long-acting anticoagulants with short-acting agents such as heparin (Hornor et al., 2018). Perioperative bridging with heparin is common practice and several protocols have been described (Douketis et al., 2004; Spyropoulos, 2010). More recently, low-molecular-weight heparin (LMWH) has become the primary bridging therapy agent, taking the place of unfractionated heparin (UFH), due to a low incidence of bleeding complications with LMWH (Dunn et al., 2007). A dose of 1 mg/kg LMWH twice daily is now standard practice.
However, bridging is recommended only for patients with a high perioperative VTE risk if anticoagulation is discontinued (Siegal et al., 2012). Patients that perioperative bridging is recommended for include those with nonvalvular atrial fibrillation and a high perioperative risk of VTE and patients with a history of stroke/embolic events, cardiac thrombus, or a CHADS2 score ≥5–6, or a CHA2DS2 VASc score of ≥6 (Hornor et al., 2018). An expert consensus defined two patient populations that should be bridged due to high VTE risk (figure 1) (Baron et al., 2013).
Figure 1. Expert consensus of two patient populations at high risk of VTE (Baron et al., 2013).
VTE, Venous thromboembolism
A summary of the recommendations for perioperative heparin bridging from the American College of Surgeons (ACS) guidelines covering antiplatelet therapy, non-vitamin K anticoagulants (NOACs) and warfarin therapy can be found in this section (Hornor et al., 2018).
Antiplatelet therapy
It is advised that patients undergoing surgical procedures that require antiplatelet cessation do not receive bridging agents due to a lack of evidence to support a benefit from antiplatelet bridging therapy (Douketis et al., 2012; Childers et al., 2018).
Non-vitamin K anticoagulant (NOAC) therapy
Due to the rapid onset of action of NOACs, and their predictable half-lives, bridging is unnecessary in the perioperative setting (Spyropoulos et al., 2016).
Warfarin therapy
Heparin bridging is almost exclusively used in high VTE-risk patients on chronic warfarin therapy, and the ACS guidelines provide a protocol for bridging these patients (figure 2). This approach is in line with the American College of Chest Physicians (ACCP) guidelines (Douketis et al., 2012)
Figure 2. Recommended bridging approach (Hornor et al., 2018).
INR, International normalised ratio; LMWH, Low-molecular-weight heparin; UFH, Unfractionated heparin
When administering heparin bridging therapy, it is important to monitor for heparin-induced thrombocytopenia, which typically presents as a drop in the platelet count, as well as monitoring for paradoxical thrombosis (Hornor et al., 2018).
The ACS guidelines so far have discussed the thromboembolic risks of stopping antithrombotic medications, the procedural bleeding risks, and the appropriateness of perioperative heparin bridging. Now these risks have been assessed, we can consider management strategies for elective and emergency surgical procedures. Learn more about the ACS recommended perioperative management strategy for elective surgery in the next section of the guidelines.
Perioperative management strategy for elective surgery
After assessing the risk of major bleeding and venous thromboembolism due to the cessation of antithrombotic medication, and the associated risk of various surgical procedures, when should you stop antithrombotic therapy perioperatively? Unfortunately, one size doesn’t fit all, and the approach to building a perioperative management strategy for antithrombotic medication should be tailored to the individual’s combination of known risks. The American College of Surgeons’ (ACS) guidelines describe several management strategies based on the type of antithrombotic medication and the level of procedural bleeding risk, you can find a summary of each of these within this section.
Heparin
Warfarin is often used to manage patients who require chronic anticoagulation. However, the long-acting anticoagulating effects of warfarin should be minimised perioperatively to avoid major bleeding risk during surgery. One method often used to avoid this increased risk of bleeding while minimising thromboembolic risk is heparin bridging, although heparin bridging should also be stopped perioperatively. The ACS guidelines recommend different time frames of holding heparin depending on the type, administration, and surgical procedure (figure 1) (Hornor et al., 2018).
Figure 1. Recommended perioperative heparin holding time (Hirsh & Raschke, 2004; Douketis et al., 2012; Hornor et al., 2018).
UFH, Unfractionated heparin
Both unfractionated and low-molecular-weight heparin can be resumed 24 hours after low-risk procedures, but it is advised to wait between 48–72 hours following high-risk procedures (Douketis et al., 2012). These time frames should be carefully considered when evaluating risks of restarting anticoagulation as resuming heparin bridging anticoagulation prematurely has been associated with major bleeding rates 4 times baseline (Dunn et al., 2007).
Warfarin
Discontinuation of warfarin perioperatively should be carried out as part of heparin bridging and it is recommended that warfarin is held 5 days before surgical procedures (Hornor et al., 2018). It is also important to consider certain patient characteristics that may affect the normalisation of the coagulation cascade time, such as age and medical conditions that require anticoagulation to a higher international normalised ratio (INR) level (White et al., 1995; Hylek et al., 2001). The INR should be checked the day before and the day of the procedure and vitamin K administered if INR is supratherapeutic. After surgery warfarin can be resumed at the previous dose 12–24 hours after surgery, and it is typical for INR to return to a therapeutic level around 5 days postoperatively (Douketis et al., 2012). You can learn more about heparin bridging and the recommended management strategy of warfarin in the heparin bridging section of the guidelines.
Non-vitamin K anticoagulants (NOACs)
For many physicians, NOACs are the preferred choice of anticoagulation due to their rapid onset of action, shorter half-lives, and more predictable pharmacology in comparison to warfarin (Hornor et al., 2018). The ACS guidelines recommend creating a perioperative management strategy that takes into account the bleeding risk of surgery, the patient’s renal function, and the anticoagulant’s pharmacodynamics. For patients with normal renal function, NOACs should be held 24–48 hours before the procedure depending on the risk of surgery (figure 2). In patients with impaired renal function, it has been advised dabigatran should be held 4 days before high-risk surgery and 2 days before low-risk surgery (Hornor et al., 2018).
Figure 2. Recommended NOAC holding time in patients with normal renal function (Doherty et al., 2017; Raval et al., 2017; Hornor et al., 2018).
NOACs, Non-vitamin K anticoagulants
When considering the optimum time to resuming NOACs postoperatively, bleeding risk of the surgery, haemostasis, and patient characteristics should all be taken into consideration. Resuming anticoagulation with NOACs should also be approached with caution due to their rapid onset; one study found that resumption of NOACs 24-hours postoperatively was associated with a 1.2% 1-month major-bleeding risk (95% CI, 0.6–2.1) (Beyer-Westendorf et al., 2014).
NOACs can be resumed 2–3 days after high-risk procedures and 1 day after low-risk procedures (Hornor et al., 2018).
Antiplatelet agents
The American College of Cardiology (ACC) and the American Heart Association (AHA) clinical practice guidelines both recommend the continued use of dual antiplatelet therapy, if possible, in patients who require surgery within 30 days of drug-eluting stent placement. If dual antiplatelet therapy is not possible, aspirin should be continued, and dual antiplatelet therapy resumed as soon as possible postoperatively (Fleisher et al., 2014). More details of stent placement can be found in the thromboembolic risk section of the ACS guidelines.
Some controversy remains over whether low-dose aspirin should be held before major non-cardiac surgery when it has been prescribed for secondary prevention in patients with a non-recent history of cardiac stent placement. The ACS guidelines recommend that aspirin, either high- or low-dose, should be held 7–10 days before high bleeding risk procedures in patients without a history of percutaneous coronary intervention. If the patient does have a recent history of percutaneous coronary intervention, the surgeon should consult the prescribing cardiologist (Hornor et al., 2018). Postoperatively aspirin should not be restarted until the bleeding risk has diminished due to its fast-acting effects on platelets (within 1 hour) (Patrono et al., 2001).
Other antiplatelet agents including clopidogrel, prasugrel, and ticagrelor should be held for 5–7 days before low and high bleeding risk procedures (Douketis et al., 2012). Similar considerations as aspirin should be made postoperatively, due to the onset of action time also being within 1 hour (Patrono et al., 2001).
Elective surgery allows for perioperative strategies that can be carried out over a number of days before the procedure, but how does the strategy differ when the clinical situation requires emergency surgery, or a patient presents with active bleeding? In the next section of the guidelines, the ACS discuss the available options for the reversal of anticoagulation and the reversal agents in development.
Antithrombotic strategies in a nonelective setting
While management strategies have been recommended in elective surgery, guidance regarding anticoagulation reversal in nonelective surgery is sparse. This is due to a lack of high-quality data with much of the evidence based on cases series and expert consensus. The American College of Surgeons’ (ACS) guidelines discuss reversal agents that may be useful in this setting; however, they don’t represent a management strategy guideline for emergency situations (Hornor et al., 2018). This section demonstrates that most antithrombotic agents can be reversed or at least mitigated by a reversal agent, antifibrinolytic, or blood product transfusion.
Non-oral anticoagulants
Protamine has been shown to successfully reverse the anticoagulant effects of UFH (figure 1).
Figure 1. Protamine administration for reversal of heparin (van Veen et al., 2011; Hornor et al., 2018).
UFH, Unfractionated heparin
One reversal agent still under investigation is ciraparantag, the synthetic molecule forms hydrogen bonds to its intended targets and has been shown to reverse the effects of heparin as well as fondaparinux, factor Xa inhibitors and dabigatran (Ansell et al., 2016; Laulicht et al., 2018).
Vitamin K antagonists
Several options are available for the reversal of vitamin K antagonists (figure 2).
Figure 2. Reversal agents for vitamin K antagonists (Watson et al., 2001; Holland & Brooks, 2006; Hornor et al., 2018).
Although FFP remains an option for the reversal of vitamin K antagonists it has its disadvantages (figure 2), and in a recent randomised controlled trial that compared FFP to 4F-PCC for reversing coagulopathy secondary to warfarin, 4F-PCC was found to be superior (Goldstein et al., 2015).
The ACS recommends administering vitamin K and 4F-PCC to patients with elevated INR secondary to warfarin and who are actively bleeding and/or require urgent surgery (Hornor et al., 2018).
Non-vitamin K oral anticoagulants
Non-vitamin K oral anticoagulants (NOACs) have become increasingly popular in recent years due to their rapid onset, shorter half-lives, and predictable pharmacodynamics (Hornor et al., 2018). NOACs may have more favourable anticoagulation effects in comparison to existing therapies, but until recently there was no specific antidote to reverse these effects in emergency cases. Idarucizumab was approved by both the FDA and EMA in 2015 for the reversal of dabigatran (Praxbind® Prescribing information, 2015; Praxbind® Summary of Product Characteristics, 2015). More recently andexanet alfa gained approval for the reversal of rivaroxaban and apixaban in the US (Andexxa® Prescribing information, 2018). Along with these antidotes, other non-specific reversal agents have been shown to successfully correct anticoagulation in patients receiving NOACs (figure 3).
Figure 3. Reversal agents currently available and in development for NOACs (Eerenberg et al., 2011; Sarode, 2012; Escolar et al., 2013; Levi et al., 2014; Wong & Keeling, 2014; Pollack et al., 2015; Zahir et al., 2015; Connolly et al., 2016; Ansell et al., 2017; Hornor et al., 2018).
3F-PCC, Three-factor prothrombin complex concentrate; 4F-PCC, Four-factor prothrombin complex concentrate
Antiplatelet agents
Platelet transfusion can be administered to patients who are receiving antiplatelet agents, such as aspirin if they have active bleeding or require emergency surgery. The emergency treatment can replace platelets with altered function due to antiplatelet therapy. However, there is very limited data surrounding the benefits and risks of administering platelet transfusion in the emergency surgery setting for patients taking antiplatelet agents. The ACS has therefore, recommended that platelets are only administered in urgent clinical situations that warrant such therapy (figure 4) (Hornor et al., 2018).
Figure 4. Recommended platelet transfusion for patients receiving antiplatelet agents (Sarode, 2012; Hornor et al., 2018)
References
American College of Surgeons
Hornor MA, Duane TM, Ehlers AP, Jensen EH, Brown PS Jr, Pohl D, et al. American College of Surgeons' Guidelines for the Perioperative Management of Antithrombotic Medication. J Am Coll Surg. 2018:227;521–36.
Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220.
Estimating thromboembolic risk
Bates SM, Greer IA, Middeldorp S, Veenstra DL, Prabulos AM, Vandvik PO. VTE, thrombophilia, antithrombotic therapy, and pregnancy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e691S–e736S.
Cannegieter SC, Rosendaal FR, Briët E. Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses. Circulation. 1994;89:635–41.
de Jong PG, Coppens M, Middeldorp S. Duration of anticoagulant therapy for venous thromboembolism: balancing benefits and harms on the long term. Br J Haematol. 2012;158:433–41.
Deviri E, Sareli P, Wisenbaugh T, Cronje SL. Obstruction of mechanical heart valve prostheses: clinical aspects and surgical management. J Am Coll Cardiol. 1991;17:646–50.
Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141:e326S–e50S.
Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. 2014;383:245–54.
Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, Bozkurt B, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014;64:e77–e137.
Friberg L, Rosenqvist M, Lip GY. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: the Swedish Atrial Fibrillation cohort study. Eur Heart J. 2012;33:1500–10.
Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135:e686–e725.
Hornor MA, Duane TM, Ehlers AP, Jensen EH, Brown PS Jr, Pohl D, et al. American College of Surgeons' Guidelines for the Perioperative Management of Antithrombotic Medication. J Am Coll Surg. 2018:227;521–36.
Iakovou I, Schmidt T, Bonizzoni E, Ge L, Sangiorgi GM, Stankovic G, Airoldi F, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005;293:2126–30.
Jørgensen ME, Torp-Pedersen C, Gislason GH, Jensen PF, Berger SM, Christiansen CB, et al. Time elapsed after ischemic stroke and risk of adverse cardiovascular events and mortality following elective noncardiac surgery. JAMA. 2014;312:269–77.
Kearon C, Ageno W, Cannegieter SC, Cosmi B, Geersing GJ, Kyrle PA, et al. Categorization of patients as having provoked or unprovoked venous thromboembolism: guidance from the SSC of ISTH. J Thromb Haemost. 2016;14:1480–3.
Kleiman NS. Grabbing the horns of a dilemma: the duration of dual antiplatelet therapy after stent implantation. Circulation. 2012;125:1967–70.
Levine MN, Hirsh J, Gent M, Turpie AG, Weitz J, Ginsberg J, et al. Optimal duration of oral anticoagulant therapy: a randomized trial comparing four weeks with three months of warfarin in patients with proximal deep vein thrombosis. Thromb Haemost. 1995;74:606–11.
Research Committee of the British Thoracic Society. Optimum duration of anticoagulation for deep-vein thrombosis and pulmonary embolism. Lancet. 1992;340:873–6.
Savonitto S, Caracciolo M, Cattaneo M, DE Servi S. Management of patients with recently implanted coronary stents on dual antiplatelet therapy who need to undergo major surgery. J Thromb Haemost. 2011;9:2133–42.
Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, Baumgartner H, et al. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J. 2012;33:2451–96.
Whitlock RP, Sun JC, Fremes SE, Rubens FD, Teoh KH. Antithrombotic and thrombolytic therapy for valvular disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e576S–e600S.
Wu C, Alotaibi GS, Alsaleh K, Linkins LA, McMurty MS. Case-fatality of recurrent venous thromboembolism and major bleeding associated with aspirin, warfarin, and direct oral anticoagulants for secondary prevention. Thromb Res. 2015;135:243–8.
Wu C, Alotaibi GS, Alsaleh K, Sean McMurtry M. Case fatality of bleeding and recurrent venous thromboembolism during, initial therapy with direct oral anticoagulants: a systematic review. Thromb Res. 2014;134:627–32.
Procedural bleeding risk
Baron TH, Kamath PS, McBane RD. Management of antithrombotic therapy in patients undergoing invasive procedures. N Engl J Med. 2013;368:2113–24.
Chee Y, Crawford J, Watson H, Greaves M. Guidelines on the assessment of bleeding risk prior to surgery or invasive procedures. Br J Haematol. 2008;140:496–504.
Hornor MA, Duane TM, Ehlers AP, Jensen EH, Brown PS Jr, Pohl D, et al. American College of Surgeons' Guidelines for the Perioperative Management of Antithrombotic Medication. J Am Coll Surg. 2018:227;521–36.
Omran H, Bauersachs R, Rübenacker S, Goss F, Hammerstingl C. The HAS-BLED score predicts bleedings during bridging of chronic oral anticoagulation. Results from the national multicentre BNK Online bRiDging REgistRy (BORDER). Thromb Haemost. 2012;108:65–73.
Roldán V, Marín F, Manzano-Fernández S, Gallego P, Vílchez JA, Valdés M, et al. The HAS-BLED score has better prediction accuracy for major bleeding than CHADS2 or CHA2DS2-VASc scores in anticoagulated patients with atrial fibrillation. J Am Coll Cardiol. 2013;62:2199–204.
Spyropoulos AC, Al-Badri A, Sherwood MW, Douketis JD. Periprocedural management of patients receiving a vitamin K antagonist or a direct oral anticoagulant requiring an elective procedure or surgery. J Thromb Haemost. 2016;14:875–85.
Tafur AJ, McBane R 2nd, Wysokinski WE, Litin S, Daniels P, Slusser J, et al. Predictors of major bleeding in peri-procedural anticoagulation management. J Thromb Haemost. 2012;10:261–7.
Veitch AM, Baglin TP, Gershlick AH, Harnden SM, Tighe R, Cairns S, et al. Guidelines for the management of anticoagulant and antiplatelet therapy in patients undergoing endoscopic procedures. Gut. 2008;57:1322–9.
Perioperative heparin bridging
Baron TH, Kamath PS, McBane RD. Management of antithrombotic therapy in patients undergoing invasive procedures. N Engl J Med. 2013;368:2113–24.
Childers CP, Maggard-Gibbons M, Ulloa JG, MacQueen IT, Miake-Lye IM, Shanman R, et al. Perioperative management of antiplatelet therapy in patients undergoing non-cardiac surgery following coronary stent placement: a systematic review. Syst Rev. 2018;7:4.
Douketis JD, Johnson JA, Turpie AG. Low-molecular-weight heparin as bridging anticoagulation during interruption of warfarin: assessment of a standardized periprocedural anticoagulation regimen. Arch Intern Med. 2004;164:1319–26.
Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Exkman MH, et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141:e326S–e350S.
Dunn AS, Spyropoulos AC, Turpie AG. Bridging therapy in patients on long-term oral anticoagulants who require surgery: the Prospective Peri-operative Enoxaparin Cohort Trial (PROSPECT). J Throm Haemost. 2007;5:2211–8.
Hornor MA, Duane TM, Ehlers AP, Jensen EH, Brown PS Jr, Pohl D, et al. American College of Surgeons' Guidelines for the Perioperative Management of Antithrombotic Medication. J Am Coll Surg. 2018:227;521–36.
Siegal D, Yudin J, Kaatz S, Douketis JD, Lim W, Spyropoulos AC. Periprocedural heparin bridging in patients receiving vitamin K antagonists: systematic review and meta-analysis of bleeding and thromboembolic rates. Circulation. 2012;126:1630–9.
Spyropoulos AC, Al-Badri A, Sherwood MW, Douketis JD. Periprocedural management of patients receiving a vitamin K antagonist or a direct oral anticoagulant requiring an elective procedure or surgery. J Thromb Haemost. 2016;14:875–85.
Spyropoulos AC. Bridging therapy and oral anticoagulation: current and future prospects. Curr Opin Hematol. 2010;17:444–9.
Perioperative management strategy for elective surgery
Beyer-Westendorf J, Gelbricht V, Förster K, Ebertz F, Köhler C, Werth S, et al. Peri-interventional management of novel oral anticoagulants in daily care: results from the prospective Dresden NOAC registry. Eur Heart J. 2014;35:1888–96.
Doherty JU, Gluckman TJ, Hucker WJ, Januzzi JL Jr, Ortel TL, Saxonhouse SJ, et al. 2017 ACC expert consensus decision pathway for periprocedural management of anticoagulation in patients with nonvalvular atrial fibrillation: a report of the American College of Cardiology Clinical Expert Consensus Document Task Force. J Am Coll Cardiol. 2017;69:871–98.
Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141:e326S–e350S.
Dunn AS, Spyropoulos AC, Turpie AG. Bridging therapy in patients on long-term oral anticoagulants who require surgery: the Prospective Peri-operative Enoxaparin Cohort Trial (PROSPECT). J Throm Haemost. 2007;5:2211–8.
Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, Bozkurt B, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014;64:e77–e137.
Hirsh J, Raschke R. Heparin and low-molecular-weight heparin: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:188S–203S.
Hornor MA, Duane TM, Ehlers AP, Jensen EH, Brown PS Jr, Pohl D, et al. American College of Surgeons' Guidelines for the Perioperative Management of Antithrombotic Medication. J Am Coll Surg. 2018:227;521–36.
Hylek EM, Regan S, Go AS, Hughes RA, Singer DE, Skates SJ. Clinical predictors of prolonged delay in return of the international normalized ratio to within the therapeutic range after excessive anticoagulation with warfarin. Ann Intern Med. 2001;135:393–400.
Patrono C, Coller B, Dalen JE, FitzGerald GA, Fuster V, Gent M, et al. Platelet-active drugs : the relationships among dose, effectiveness, and side effects. Chest. 2001;119:39S–63S.
Raval AN, Cigarroa JE, Chung MK, Diaz-Sandoval LJ, Diercks D, Piccini JP, et al. Management of patients on non-vitamin K antagonist oral anticoagulants in the acute care and periprocedural setting: A scientific statement from the American Heart Association. Circulation. 2017;135:e604–e633.
White RH, McKittrick T, Hutchinson R, Twitchell J. Temporary discontinuation of warfarin therapy: changes in the international normalized ratio. Ann Intern Med. 1995;122:40–2.
Antithrombotic strategies in a nonelective setting
Andexxa® Prescribing information. 2018. Available at https://www.fda.gov/downloads/BiologicsBloodVaccines/CellularGeneTherapyProducts/ApprovedProducts/UCM606687.pdf (accessed January 2019).
Ansell JE, Bakhru SH, Laulicht BE, Steiner SS, Grosso MA, Brown K, et al. Single-dose ciraparantag safely and completely reverses anticoagulant effects of edoxaban. Thromb Haemost. 2017;117:238–45.
Ansell JE, Laulicht BE, Bakhru SH, Hoffman M, Steiner SS, Costin JC. Ciraparantag safely and completely reverses the anticoagulant effects of low molecular weight heparin. Thromb Res. 2016;146:113–8.
Connolly SJ, Milling TJ Jr, Eikelboom JW, Gibson CM, Curnutte JT, Gold A, et al. Andexanet Alfa for acute major bleeding associated with Factor Xa inhibitors. N Engl J Med. 2016;375:1131–41.
Eerenberg ES, Kamphuisen PW, Sijpkens MK, Meijers JC, Buller HR, Levi M. Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: a randomized, placebo-controlled, crossover study in healthy subjects. Circulation. 2011;124:1573–9.
Escolar G, Fernandez-Gallego V, Arellano-Rodrigo E, Roquer J, Reverter JC, Sanz VV, et al. Reversal of apixaban induced alterations in hemostasis by different coagulation factor concentrates: significance of studies in vitro with circulating human blood. PLoS One. 2013;8:e78696.
Goldstein JN, Refaai MA, Milling TJ Jr, Lewis B, Goldberg-Alberts R, Hug BA, et al. Four-factor prothrombin complex concentrate versus plasma for rapid vitamin K antagonist reversal in patients needing urgent surgical or invasive interventions: a phase 3b, open-label, non-inferiority, randomised trial. Lancet. 2015;385:2077–87.
Holland LL, Brooks JP. Toward rational fresh frozen plasma transfusion: The effect of plasma transfusion on coagulation test results. Am J Clin Pathol. 2006;126:133–9.
Hornor MA, Duane TM, Ehlers AP, Jensen EH, Brown PS Jr, Pohl D, et al. American College of Surgeons' Guidelines for the Perioperative Management of Antithrombotic Medication. J Am Coll Surg. 2018:227;521–36.
Laulicht B, Bakhru S, Lee C, Baker C, Jiang X, Mathiowitz E, et al. Abstract 11395: Small molecule antidote for anticoagulants. Circulation. 2018;126:A11395.
Levi M, Moore KT, Castillejos CF, Kubitza D, Berkowitz SD, Goldhaber SZ, et al. Comparison of three-factor and four-factor prothrombin complex concentrates regarding reversal of the anticoagulant effects of rivaroxaban in healthy volunteers. J Thromb Haemost. 2014;12:1428–36.
Pollack CV Jr, Reilly PA, Eikelboom J, Glund S, Verhamme P, Bernstein RA, et al. Idarucizumab for dabigatran reversal. N Engl J Med. 2015;373:511–20.
Praxbind® Prescribing information. 2015. Available at https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/761025lbl.pdf (accessed January 2019).
Praxbind® Summary of Product Characteristics. 2015. Available at https://www.ema.europa.eu/en/medicines/human/EPAR/praxbind#authorisation-details-section (accessed January 2019).
Sarode R. How do I transfuse platelets (PLTs) to reverse anti-PLT drug effect? Transfusion. 2012;52:695–701.
Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, Baumgartner H, et al. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J. 2012;33:2451–96.
van Veen JJ, Maclean RM, Hampton KK, Laidlaw S, Kitchen S, Toth P, et al. Protamine reversal of low molecular weight heparin: clinically effective? Blood Coagul Fibrinolysis. 2011;22:565–70.
Watson HG, Baglin T, Laidlaw SL, Makris M, Preston FE. A comparison of the efficacy and rate of response to oral and intravenous Vitamin K in reversal of over-anticoagulation with warfarin. Br J Haematol. 2001;115:145–9.
Wong H, Keeling D. Activated prothrombin complex concentrate for the prevention of dabigatran-associated bleeding. Br J Haematol. 2014;166:152–3.
Zahir H, Brown KS, Vandell AG, Desai M, Maa JF, Dishy V, et al. Edoxaban effects on bleeding following punch biopsy and reversal by a 4-factor prothrombin complex concentrate. Circulation. 2015;131:82–90.
of interest
are looking at
saved
next event
Job number: KCT16-01-0010
Developed by EPG Health for Medthority in collaboration with CSL Behring, with content provided by CSL Behring.
Not intended for Healthcare Professionals outside Europe.

